Articles
- Page Path
- HOME > Kosin Med J > Volume 37(1); 2022 > Article
-
Original article
Validation of the association of the cystic duct fibrosis score with surgical difficulty in laparoscopic cholecystectomy -
Hyung Hwan Moon
 , Ji Hoon Jo
, Ji Hoon Jo , Young Il Choi
, Young Il Choi , Dong Hoon Shin
, Dong Hoon Shin
-
Kosin Medical Journal 2022;37(1):61-67.
DOI: https://doi.org/10.7180/kmj.21.049
Published online: March 15, 2022
Department of Surgery, Kosin University Gospel Hospital, Kosin University College of Medicine, Busan, Korea
- Corresponding Author: Young Il Choi, MD, PhD Department of Surgery, Kosin University Gospel Hospital Kosin University College of Medicine, 262 Gamcheon-ro, Seo-gu, Busan 49267, Korea Tel: +82-51-990-3005 Fax: +82-51-990-6462 E-mail: tsojc@naver.com
Copyright © 2022 Kosin University College of Medicine.
This is an open-access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
- 2,038 Views
- 51 Download
- 1 Crossref
Abstract
-
Background
- The level of surgical difficulty in laparoscopic cholecystectomy might be predictable based on preoperative imaging and intraoperative findings indicative of cholecystitis severity. Several scales for laparoscopic cholecystectomy have been developed, but most are complex, unverified, and not widely adopted. This study evaluated the association of the cystic duct fibrosis score (range, 0–3) with surgical difficulty in laparoscopic cholecystectomy.
-
Methods
- Between July 2018 and November 2018, 163 laparoscopic cholecystectomy cases were retrospectively reviewed at a single center. Patients’ demographics, preoperative laboratory data, operation time, complications, hospital stay, and cholecystitis severity grade were investigated. We also evaluated the associations of the Tokyo Guidelines 2018 and the Parkland grading scale with the cystic fibrosis score.
-
Results
- The cystic duct fibrosis score was associated with preoperative white blood cells (p<0.001), preoperative platelet count (p=0.046), preoperative total bilirubin (p<0.004), preoperative C-reactive protein (p<0.001), operation time (p<0.001), cystic duct ligation time (p=0.002), estimated blood loss (p<0.001), postoperative complication (p=0.004), open conversion (p<0.001), and common bile duct injury (p=0.010). The cystic duct fibrosis score was also correlated with the Tokyo Guidelines 2018 and the Parkland grading scale (p<0.001). The cystic duct ligation time predicted the cystic duct fibrosis score and the Parkland grading scale, but not the Tokyo Guidelines 2018.
-
Conclusion
- As a simple indicator of cholecystitis severity, the cystic duct fibrosis score can predict the surgical difficulty and outcomes of laparoscopic cholecystectomy.
- Laparoscopic cholecystectomy (LC) is the gold-standard treatment of benign gallbladder (GB) disease, and one of the most common laparoscopic surgery [1,2]. However, inflammation of the GB is known to make surgery difficult, and increase postoperative complications [3,4]. There are several studies on the degree of GB inflammation, difficulty of surgery, and prediction of postoperative complications and progress in patients with LC [5-7]. Among many studies, Tokyo Guidelines 2018 (TG 18) and Parkland grading scale (PGS) are representative methods based on factors including preoperative symptoms, imaging, blood test, and intraoperative findings for the severity of acute cholecystitis (AC) [8-10].
- However, sometimes the degree of cholecystitis based on preoperative images, symptoms, and blood tests are quite different from actual difficulties in surgery [11]. The most important part of LC is establishing a critical view of safety (CVS), cystic duct isolation, and ligation [12]. We assume that the degree of inflammation of the cystic duct will affect the technical difficulties of LC. We scored the hardness of the cystic duct as a cystic duct fibrosis score (CFS). This study aimed to validate the CFS as a predictor of surgical difficulty in LC and compare CFS with TG 18 and PGS
Introduction
- Ethical statements: The protocol was approved by the Kosin University Gospel Hospital Institutional Review Board (KUGH 2021-10-019). The informed consent was waived because this design is a retrospective study.
- 1. Study population
- Between July 2018 and November 2018, 165 cases of LC were retrospectively reviewed in a single tertiary medical center. We analyzed demographics, preoperative laboratory data, operation time, complications according to Clavien-Dindo classification, hospital stay, and severity grade of AC. In addition, we graded TG 18, PGS, and CFS, and compared preoperative, intraoperative, and postoperative parameters according to CFS grade. Moreover, we evaluated the association among TG 18, PSG, and CFS.
- 2. Surgical procedure
- LC was performed by four hepato-biliary surgeons. The patients who had previously undergone open upper abdominal surgery or underwent single port LC were excluded. The GB is retracted over the liver with cephalic traction. The dissection begins with an incision of the peritoneum on both sides of GB to open up the hepatocystic triangle. After establishing CVS, the cystic duct and the cystic artery were isolated, ligated, and cut. Retrograde dissection of the GB from the liver bed is performed. If it was difficult to accurately identify the CVS, the fundus first approach was performed.
- 3. Definition
- TG 18 diagnostic criteria were used for disease severity in patients with AC [13]. The grading system is as follows: I (mild AC), II (moderate AC), and III (severe AC). Information regarding patient medical history, physical examination, ultrasound findings, and laboratory values (white blood cell count, international normalized ratio, and complete blood cell count), as well as vasopressor use or mechanical ventilator status, were abstracted [14]. If there was no AC, we graded it as 0.
- The appearance of GB was graded by the surgeon’s description as PGS intraoperatively [10]: 1, normal appearing GB (“robin's egg blue”); 2, minor adhesions at the neck, otherwise normal GB; 3, hyperemia, pericholecystic fluid, adhesions to the body, distended GB; 4, adhesions obscuring the majority of GB or grade I-III with abnormal liver anatomy, intrahepatic GB, or impacted stone (Mirrizi syndrome); or 5, perforation, necrosis, inability to visualize the GB due to adhesions [10].
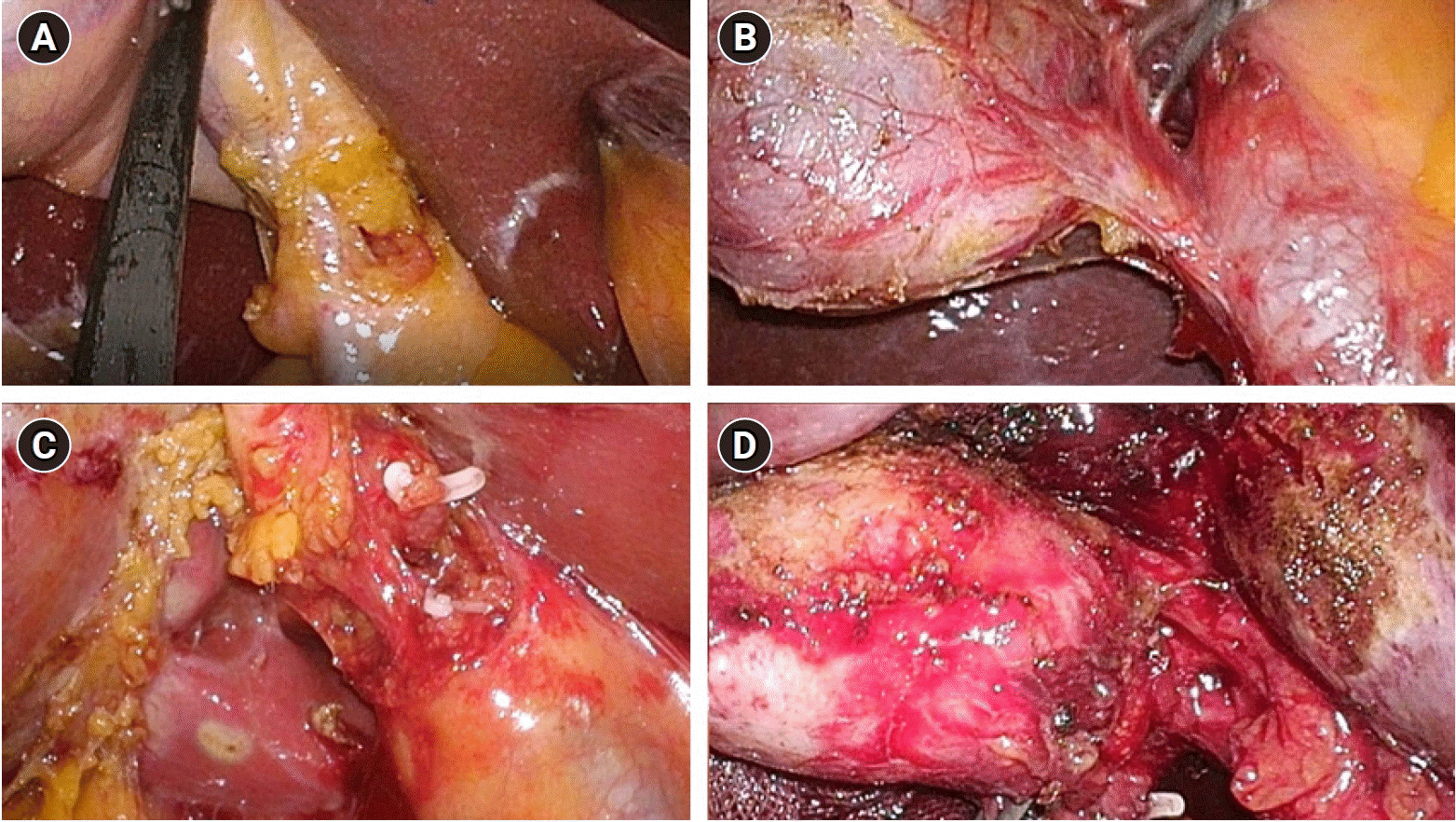
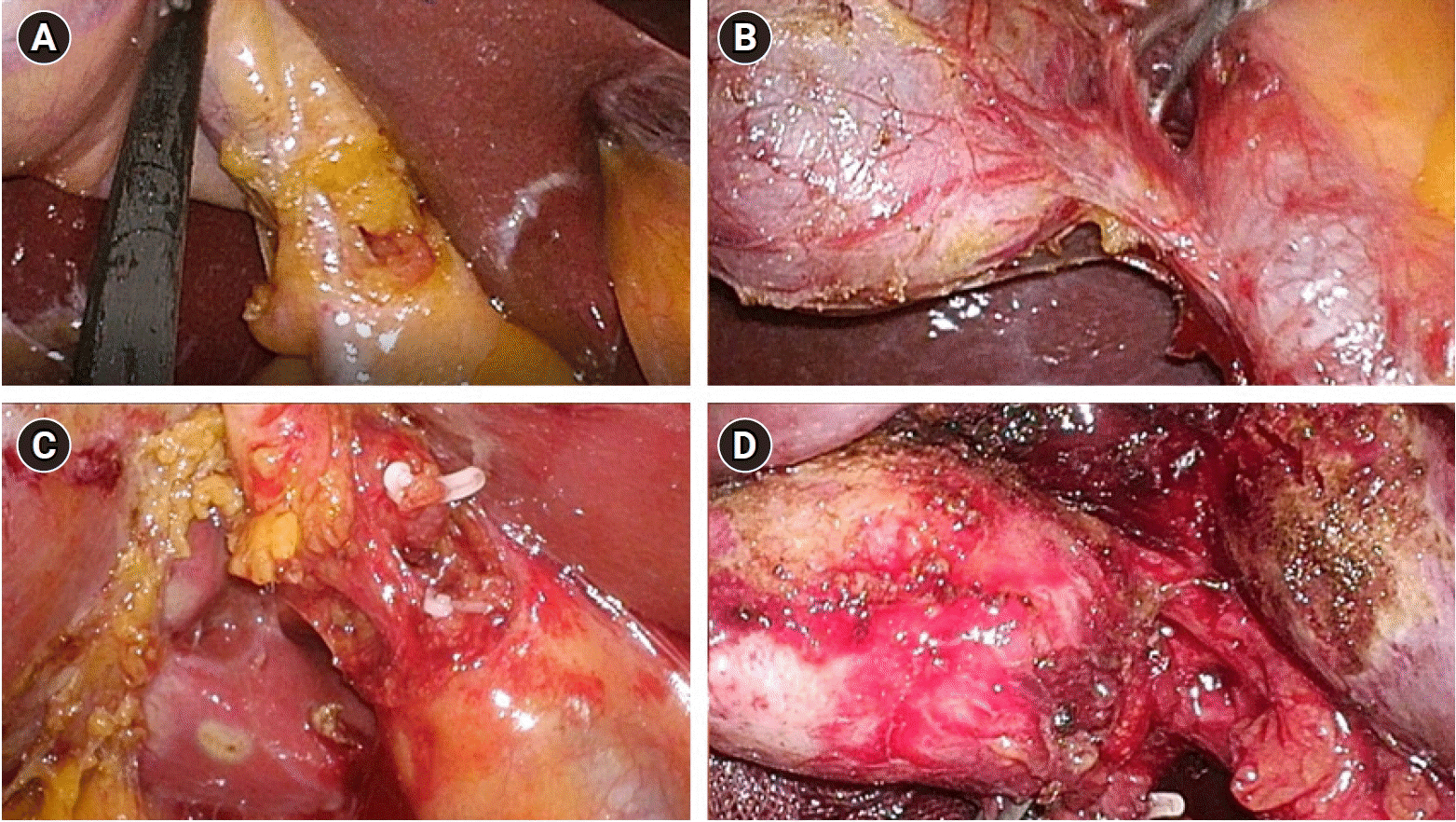
- CFS was classified and scored by surgeon’s description when dissecting a cystic duct (Fig. 1): 0, normal or no inflammation; 1, edematous but not hard; 2, not easy to dissect the cystic duct due to partial hardness (less than 50%); or 3, hard to dissect the cystic duct due to whole hardness (more than 50%).
- Cystic duct ligation time was minutes from the start of surgery to the cystic duct ligation with clip or stapler. Clavien-Dindo classification II or more was defined as postoperative complications.
- 4. Statistics
- Data included demographics, preoperative laboratory data, operation time, complications according to Clavien-Dindo classification, hospital stay, and severity grade of AC. The chi-square test was used to compare categorical variables. One-way analysis of variance test for independent samples was used to compare continuous variables. Continuous variables are presented as means with standard deviations. Linear by linear association was used to compare categorical variables among the CFS grade. Univariate linear regression was used for the analysis of the relation between cystic duct ligation time and operation time among severity grades of cholecystitis. In all analyses, a p-value of <0.05 was regarded as statistically significant. SPSS version 22.0 (IBM Corp., Armonk, NY, USA) was used for statistical analysis in the present study.
Methods
- 1. Demographics
- A total of 85 males and 78 females were included in this study, their mean age was 56.6 years. the mean body mass index was 25.0 kg/m2, the mean preoperative white blood cell (WBC) was 7,850 μL, the mean preoperative C-reactive protein (CRP) was 2.742 mg/dL. Eighty-one percent of them have gallstones and GB wall thickening was shown on computed tomography in 45.4% of them. In 31.9% of them needed preoperative percutaneous GB drainage. The mean operative time was 62.1 minutes and the hospital stay was 5.4 days. There were five cases of open conversion common bile duct (CBD) injury had happened in two cases during a laparoscopic procedure, we converted open surgery and inserted T-tube in CBD. The other case was difficult to proceed LC due to severe inflammation of GB. Postoperative complications included wound seroma, infection, and diarrhea (Clavien-Dindo II), one case of bile leak from CBD (Clavien-Dindo III) (Table 1).
- 2. Comparison of characteristics according to CFS
- We compared the patient's characteristics according to CFS (Table 2). The higher CFS was associated with older patients (p=0.005), longer operative time (p<0.001) and cystic duct ligation time (p=0.002). Additionally, higher preoperative WBC (p<0.001) and CRP (p<0.001), lower preoperative platelet count (p=0.046), more estimated blood loss (p<0.001), high American Society of Anesthesiologists score (p=0.001), more GB stones (p=0.029), GB wall thickening (p<0.001), preoperative intervention (p<0.001), open conversion (p<0.001), CBD injury (p=0.010), and postoperative complications (p=0.004) in the higher CFS statistical significantly.
- 3. Associations of operative time and cystic duct ligation time with severity grade of cholecystitis
- We analyzed the association among severity grades of AC with TG 18, PGS, and CFS. CFS is correlated well with TG 18, PGS (p<0.001) (Table 3). All three systems are well predicted the overall operation time of LC (p<0.001) (Table 4). In addition, it was analyzed that the cystic duct ligation time was well predicted in CFS and PGS except TG 18.
Results
- This study validated the CFS during LC and compared it with TG 18 and PGS CFS is a good predictor of the severity of AC through a comparison of preoperative laboratory data according to CFS; preoperative WBC (p<0.001), preoperative platelet (p=0.046), preoperative total bilirubin (p<0.004), and preoperative CRP (p<0.001). Through this, we can assume that CFS will be high during surgery if the preoperative inflammation-related laboratory data is severe.
- In addition, CFS is a good predictor of the difficulty of LC, postoperative outcomes; operative time (p<0.001), cystic duct ligation time (p=0.002), estimated blood loss (p<0.001), postoperative complication (p=0.004), open conversion (p<0.001), and CBD injury (p=0.010). Therefore, if the CFS is high during surgery, there is a high possibility of complications during or after surgery, so be careful. In addition, we expected that the operation time and hospital stay might be longer. Moreover, it was possible to confirm the predictive ability of CFS once more through that CFS matches TG 18 (p<0.001) and PGS (p<0.001).
- There are many grading methods to measure the severity of AC. These methods allow us to anticipate difficulties in surgery and predict postoperative results and complications and help us predict possible postoperative courses [7,8,10,14]. TG 18 is well known diagnostic criterion for the management of AC [15]. TG 18 is based on the preoperative symptom, blood test, radiologic findings, and presence of organ failure [16]. However, there is a limitation to predicting the difficulty of surgery with a TG 18 grade itself [14,17]. Moreover, the difficulty scoring of TG 18 listed 25 items that have 0 to 6 points [12]. The complemented scoring system is considered too complex to be applied clinically. In contrast to TG 18, Sugrue et al. [7] established a new scoring system, using operative findings such as GB appearance, distension, adhesion, or impacted stone of the GB during surgery. This is the first introduced classification of AC with intraoperative findings. However, These scoring systems are also complex, with multiple inputs and grades, limiting the practicality of using these scores during operation.
- The American Association for the Surgery of Trauma (AAST) developed a grading system for AC as I to V. Individualized anatomically driven injury patterns were used in AAST grading for assessment of AC [14]. AAST grade was validated and reported to be superior to TG 18 in the prediction of postoperative mortality, complications, and the need for preoperative GB drainage [14]. The weakness of AAST grade is no significant differences in clinical events were noted between AAST grades 1 and 2 cholecystitis [18].
- Meanwhile, PGS is simple, intuitive, and easy reproducible among surgeons when compared to a previous grading system based on intraoperative findings [10]. PGS is classified as the degree of inflammation of GB with the level of adhesion and covering of omentum on GB [10]. PGS was demonstrated that higher grades have a longer operative time, increased operative difficulty, and increased postoperative complication rate compared to lower grades [11]. However, even though grade 5, after peeling off omentum covering GB, the operation would be easier due to less inflammation than expected in some cases. Securing CVS is one of the most important processes in LC. The difficulty of this process is directly linked to postoperative complications including bile duct injury.
- We evaluated cystic duct fibrosis because the harder the cystic duct, the more difficult to secure CVS [2,5]. Then it results in prolonged surgery, bailout procedure, unexpected bleeding, and possible bile duct, vessel, or other organ injuries [12]. TG 18 mentioned a fibrotic change in the Calot’s triangle area as one of the difficulty scores for intraoperative findings [12]. But we grade cystic duct fibrosis and hypothesized CFS itself is related to surgical difficulty and postoperative outcomes. This study shows CFS is related to the severity of cholecystitis and the surgical difficulty of LC. Of course, it is difficult to detect the degree of AC and predict the difficulty of surgery by CFS alone. If too many details are included, it becomes a complex system and becomes difficult to apply in practice [19,20].
- We acknowledge this study has several limitations. First, the proportion of patients of cholecystectomy was relatively small from a single institution. Second, the cystic duct is hidden by the peritoneum or covered with omentum in AC. Therefore, before peeling off adhesion tissue or incision of the peritoneum, accurate evaluation of cystic duct fibrosis is limited. Third, CFS has aspects of subjective assessment depending on the surgeon. In addition, surgical skills and policies of treatment may vary depending on the surgeon. Nevertheless, CFS is significantly correlated well with the severity of AC, operation time, cystic duct ligation time, hospital stay, and complications. In addition, CFS is well-matched with TG 18 and PGS. CFS could be used as a simple predictor of severity of AC and difficulty of LC and postoperative outcomes.
Discussion
-
Conflicts of interest
Young Il Choi is an editorial board member of the journal but was not involved in the peer reviewer selection, evaluation, or decision process of this article. No other potential conflicts of interest relevant to this article were reported.
-
Funding
None.
-
Author contributions
Conceptualization: HHM, YIC, DHS. Data curation: HHM, YIC. Methodology: HHM. Writing- original draft: HHM, JHJ, YIC. Writing- review & editing: JHJ, YIC, DHS. Approval of final manuscript: all authors.
Article information
Values are presented as mean±standard deviation, number (%), or number only.
BMI, body mass index; WBC, white blood cell; CRP, C-reactive protein; TG 18, Tokyo Guidelines 2018; PGS, Parkland grading scale; CFS, cystic duct fibrosis score; PTGBD, percutaneous transhepatic gallbladder drainage; ERBD, endoscopic retrograde biliary drainage; CBD, common bile duct.
Score 0, normal or no inflammation; score 1, edematous but not hard; score 2, not easy to dissect the cystic duct due to partial hardness (less than 50%); score 3, hard to dissect the cystic duct due to whole hardness (more than 50%).
BMI, body mass index; WBC, white blood cell; TB, total bilirubin; CRP, C-reactive protein; ASA, American Society of Anesthesiologists; TG 18, Tokyo Guidelines 2018; PGS, Parkland grading scale; GB, gallbladder; PTGBD, percutaneous transhepatic gallbladder drainage; ERBD, endoscopic retrograde biliary drainage; C-D, Clavien-Dindo classification; CBD, common bile duct.
| p-value | |||
|---|---|---|---|
| Tokyo Guideline 2018 | Parkland grading scale | Cystic fibrosis score | |
| Tokyo Guideline 2018 | - | 0.001 | 0.001 |
| Parkland grading scale | 0.001 | - | 0.001 |
| Cystic fibrosis score | 0.001 | 0.001 | - |
- 1. Bekki T, Abe T, Amano H, Hanada K, Kobayashi T, Noriyuki T, et al. Validation of the Tokyo guideline 2018 treatment proposal for acute cholecystitis from a single-center retrospective analysis. Asian J Endosc Surg 2021;14:14–20.ArticlePubMed
- 2. Iwashita Y, Hibi T, Ohyama T, Honda G, Yoshida M, Miura F, et al. An opportunity in difficulty: Japan-Korea-Taiwan expert Delphi consensus on surgical difficulty during laparoscopic cholecystectomy. J Hepatobiliary Pancreat Sci 2017;24:191–8.ArticlePubMed
- 3. Yokoe M, Takada T, Hwang TL, Endo I, Akazawa K, Miura F, et al. Validation of TG13 severity grading in acute cholecystitis: Japan-Taiwan collaborative study for acute cholecystitis. J Hepatobiliary Pancreat Sci 2017;24:338–45.ArticlePubMed
- 4. Inoue K, Ueno T, Douchi D, Shima K, Goto S, Takahashi M, et al. Risk factors for difficulty of laparoscopic cholecystectomy in grade II acute cholecystitis according to the Tokyo guidelines 2013. BMC Surg 2017;17:114.ArticlePubMedPMC
- 5. Iwashita Y, Ohyama T, Honda G, Hibi T, Yoshida M, Miura F, et al. What are the appropriate indicators of surgical difficulty during laparoscopic cholecystectomy? Results from a Japan-Korea-Taiwan multinational survey. J Hepatobiliary Pancreat Sci 2016;23:533–47.ArticlePubMed
- 6. Ansaloni L, Pisano M, Coccolini F, Peitzmann AB, Fingerhut A, Catena F, et al. 2016 WSES guidelines on acute calculous cholecystitis. World J Emerg Surg 2016;11:25.PubMedPMC
- 7. Sugrue M, Sahebally SM, Ansaloni L, Zielinski MD. Grading operative findings at laparoscopic cholecystectomy: a scoring system. World J Emerg Surg 2015;10:14.ArticlePubMedPMC
- 8. Okamoto K, Suzuki K, Takada T, Strasberg SM, Asbun HJ, Endo I, et al. Tokyo Guidelines 2018: flowchart for the management of acute cholecystitis. J Hepatobiliary Pancreat Sci 2018;25:55–72.PubMed
- 9. Takada T. Tokyo Guidelines 2018: updated Tokyo Guidelines for the management of acute cholangitis/acute cholecystitis. J Hepatobiliary Pancreat Sci 2018;25:1–2.ArticlePubMed
- 10. Madni TD, Leshikar DE, Minshall CT, Nakonezny PA, Cornelius CC, Imran JB, et al. The Parkland grading scale for cholecystitis. Am J Surg 2018;215:625–30.ArticlePubMed
- 11. Madni TD, Nakonezny PA, Barrios E, Imran JB, Clark AT, Taveras L, et al. Prospective validation of the Parkland grading scale for cholecystitis. Am J Surg 2019;217:90–7.ArticlePubMed
- 12. Wakabayashi G, Iwashita Y, Hibi T, Takada T, Strasberg SM, Asbun HJ, et al. Tokyo Guidelines 2018: surgical management of acute cholecystitis: safe steps in laparoscopic cholecystectomy for acute cholecystitis (with videos). J Hepatobiliary Pancreat Sci 2018;25:73–86.PubMed
- 13. Palareti G, Legnani C, Cosmi B, Antonucci E, Erba N, Poli D, et al. Comparison between different D-Dimer cutoff values to assess the individual risk of recurrent venous thromboembolism: analysis of results obtained in the DULCIS study. Int J Lab Hematol 2016;38:42–9.PubMed
- 14. Hernandez M, Murphy B, Aho JM, Haddad NN, Saleem H, Zeb M, et al. Validation of the AAST EGS acute cholecystitis grade and comparison with the Tokyo guidelines. Surgery 2018;163:739–46.ArticlePubMed
- 15. Fujii Y, Ohuchida J, Chijiiwa K, Yano K, Imamura N, Nagano M, et al. Verification of Tokyo Guidelines for diagnosis and management of acute cholangitis. J Hepatobiliary Pancreat Sci 2012;19:487–91.ArticlePubMed
- 16. Yokoe M, Takada T, Strasberg SM, Solomkin JS, Mayumi T, Gomi H, et al. New diagnostic criteria and severity assessment of acute cholecystitis in revised Tokyo Guidelines. J Hepatobiliary Pancreat Sci 2012;19:578–85.ArticlePubMedPMC
- 17. Joseph B, Jehan F, Dacey M, Kulvatunyou N, Khan M, Zeeshan M, et al. Evaluating the relevance of the 2013 Tokyo Guidelines for the diagnosis and management of cholecystitis. J Am Coll Surg 2018;227:38–43.ArticlePubMed
- 18. Vera K, Pei KY, Schuster KM, Davis KA. Validation of a new American Association for the Surgery of Trauma (AAST) anatomic severity grading system for acute cholecystitis. J Trauma Acute Care Surg 2018;84:650–4.ArticlePubMed
- 19. Vivek MA, Augustine AJ, Rao R. A comprehensive predictive scoring method for difficult laparoscopic cholecystectomy. J Minim Access Surg 2014;10:62–7.ArticlePubMedPMC
- 20. Schuster KM, O'Connor R, Cripps M, Kuhlenschmidt K, Taveras L, Kaafarani HM, et al. Multicenter validation of the American Association for the Surgery of Trauma grading scale for acute cholecystitis. J Trauma Acute Care Surg 2021;90:87–96.ArticlePubMed
References
Figure & Data
References
Citations

- Correlation Between Preoperative Ultrasonography and Parkland Grading Scale in Patients Undergoing Laparoscopic Cholecystectomy
Burak Uçaner, Doğuş Durmuş, Mehmet Zeki Buldanlı, Oğuz Hançerlioğulları
Indian Journal of Surgery.2024; 86(1): 160. CrossRef

 KOSIN UNIVERSITY COLLEGE OF MEDICINE
KOSIN UNIVERSITY COLLEGE OF MEDICINE
 PubReader
PubReader ePub Link
ePub Link Cite
Cite