Articles
- Page Path
- HOME > Kosin Med J > Volume 38(4); 2023 > Article
-
Original article
Initial experience with Retzius-sparing robot-assisted radical prostatectomy compared to the conventional method: is it a suitable option for robotic prostatectomy beginners? -
Su Hwan Kang

-
Kosin Medical Journal 2023;38(4):267-273.
DOI: https://doi.org/10.7180/kmj.23.143
Published online: November 9, 2023
Department of Urology, Kosin University Gospel Hospital, Kosin University College of Medicine, Busan, Korea
- Corresponding Author: Su Hwan Kang, MD Department of Urology, Kosin University College of Medicine, 262 Gamcheon-ro, Seo-gu, Busan 49267, Korea Tel: +82-51-990-5077 Fax: +82-51-990-3994 E-mail: ggangst@naver.com
• Received: August 17, 2023 • Revised: September 14, 2023 • Accepted: September 27, 2023
Copyright © 2023 Kosin University College of Medicine.
This is an open-access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
- 559 Views
- 14 Download
Abstract
-
Background
- Retzius-sparing robot-assisted radical prostatectomy (rsRARP) is a surgical procedure that can minimize the resection of surrounding prostate tissue by enabling access through the anterior surface of the Douglas pouch. We reported our initial experiences with rsRARP compared to conventional robot-assisted radical prostatectomy (RARP).
-
Methods
- Retrospective data were collected from March 2019 to June 2022, including 69 patients who underwent robotic radical prostatectomy for localized prostate cancer. The operations were performed at a single center, and we alternated between the two methods. Perioperative characteristics and oncologic and functional outcomes were analyzed.
-
Results
- In total, 35 patients underwent RARP and 34 patients underwent rsRARP. The preoperative characteristics of the patients were similar. Oncologic and functional parameters were analyzed postoperatively. Except for early recovery of urinary incontinence (immediate, 1 month, 3 months, 6 months: p<0.001, p=0.002, p=0.004, and p=0.014, respectively), there were no significant differences between the two groups. We also analyzed trends in operation time and oncologic and functional outcomes according to the progression of rsRARP cases.
-
Conclusions
- rsRARP has the major advantage of enabling an early recovery from urinary incontinence after surgery, and it is also a good surgical approach that shows oncologically similar results to the conventional approach. It is also highly reproducible and can be recommended to surgeons new to robotic radical prostatectomy.
- Since laparoscopic radical prostatectomy was first described by Schuessler in 1992, the most popular surgical approach to prostate cancer today involves making an incision toward the anterior wall of the bladder to access the anterior wall of the prostate for removal [1].
- In 2000, Binder and Kramer [2] and Abbou et al. [3] first performed and reported on robot-assisted radical prostatectomy (RARP). As the procedure evolved, it became possible to overcome its previous difficulties. Since then, robotic surgery has become the main surgical option for localized prostate cancer due to advances in anatomical understanding and techniques, such as bladder neck preservation, nerve-sparing techniques, and prostate apex management. This also made it easier to resect the prostate and re-anastomose of the urethra, which is difficult to access with a laparoscopic approach. As technology advances, interest in surgical outcomes has increased, three important factors in the surgical outcome of prostate cancer were proposed around 2005: cancer control, continence, and potency [4]. After 24 months, the proportion of participants that satisfied all three was reported to range from 50% to 60%. It is not easy to achieve both satisfactory oncological and functional results; nevertheless, steady attempts have been made to achieve both in patients with prostate cancer.
- In 2010, Galfano et al. [5] announced a new approach to robotic prostatectomy. The Retzius-sparing RARP (rsRARP) accesses the prostate through the Douglas pouch. The surgeon begins dissecting from the prostate base around the seminal vesicle without resecting any of the anterior compartment of the bladder or the prostate. This preserves the neurovascular bundle, endopelvic fascia, Aphrodite's veil, Santorini plexus, and pubourethral ligaments, which the authors argue provides a better functional outcome.
- In 2014, Lim et al. [6] published a study comparing the initial experience of rsRARP with conventional RARP and reported that the oncological results were not significantly different from those of conventional techniques, showing only advantages in reducing console time and early recovery of continence. Therefore, we reported on the initial experience and outcomes of rsRARP compared with conventional method.
Introduction
- Ethical statements: The study was approved by the Institutional Review Board (IRB) of Kosin Medical Center (IRB No: KUGH 2023-06-015). Informed consent was waived.
- 1. Participants and trial design
- From March 2019 to June 2022, the medical records of 69 patients who were diagnosed with localized prostate cancer who underwent RARP were reviewed retrospectively. Prostate cancer was confirmed preoperatively by prostate biopsy. Patients with metastases in subsequent examinations and previous transurethral prostate surgery were excluded from the study. The rsRARP was performed by a surgeon with fewer than 10 robotic prostatectomy cases in a single center. Prior to surgery, the patient underwent a complete blood count, magnetic resonance imaging of the prostate, bone scan, etc. The length of hospital stay followed our protocol, and the Foley catheter was generally removed 1 week after surgery. Age, initial prostate-specific antigen (PSA), D’Amico risk group, biopsy Gleason score, console time, estimated blood loss, pathologic stage, pathologic Gleason score, postoperative complications (Clavien-Dindo classification), postoperative continence, potency, positive surgical margin (PSM), and biochemical recurrence (BCR) were evaluated.
- 2. Definition
- Since total operative time includes time taken for other tasks, such as anesthesia and patient preparation, console time was easier to compare and also more accurate. Complications were classified according to the Clavien-Dindo system. Recovery of urinary continence was determined when the patient no longer required incontinence pads. Follow-up was immediate and then 1 month, 3 months, 6 months, and 12 months after catheter removal. Potency was defined as being able to erect sufficiently for insertion. BCR was evaluated 1 year after surgery and was diagnosed when the PSA was elevated above 0.4 ng/mL.
- 3. Surgical technique
- The surgeons had experience with several conventional methods, including open radical prostatectomy and laparoscopic-assisted radical prostatectomy. RARP was performed when the robot was introduced to our hospital in May 2017, and rsRARP was first performed in March 2019. There was no difference in the surgical method between the previously performed laparoscopic-assisted radical prostatectomy and conventional RARP, and it was performed based on the method of Menon et al. [7]. However, ligation of the vas deferens through the anterior portion of the Douglas pouch and dissection of the seminal vesicle were performed first before the anterior bladder dissection. Meanwhile, rsRARP was performed for the first time by another surgeon who had only a few RARP cases. The Retzius-sparing technique was performed with reference to the Galfano approach and Rha’s live surgery in 2018 [5,6]. The rsRARP method included the following modifications.
- The patient was placed in a standard 30º Trendelenburg position under general anesthesia. A four-arm Da Vinci robot Xi (Intuitive Surgical) was used. The patient cart was accessed from the bottom of the table or the left side of the patient. There was no difference in difficulty of the operation according to location of the patient cart. Five total trocars were used; the one for the laparoscope was placed horizontally within the umbilicus. The four robot trocars were 7 mm in diameter; one right and two left trocars were positioned at 7-cm intervals from the left and right relative to the camera port in the umbilicus. The assist port was positioned to the right side of the robot port as a 12-mm diameter port and was used for suction and traction, insertion and removal of suture material, and insertion of a specimen bag. The Prograsp, Maryland bipolar forceps, and monopolar curved scissors were inserted from the left into the robot port.
- The sigmoid colon was moved toward the head, and the bladder was pushed upward to expose the Douglas space more clearly. The parietal peritoneum above the seminal vesicles was incised horizontally. Both seminal vesicles and the vas deferens were separated and then isolated and ligated. The Denonvilliers’ fascia and the posterior fascia of the prostate were then dissected posterolaterally and the dissection continued to the apex of the prostate. To ensure nerve preservation during this process, it is important to avoid excessive instrument pressure to preserve the neurovascular bundle; dissection was also performed using a clip or Hem-o-lok.
- During the lateral dissection, the intrafascial plane was exfoliated along the contour of the prostate. In the extrafascial plane, the levator ani muscle was used as a landmark. After that, the bladder neck and the prostate base were sufficiently separated, and the bladder neck was incised at the 6 o’clock position.
- After dissection of the bladder neck, the anterior surface of the prostate was separated from the bladder. Minimal dissection of the bladder was achieved, and the Santorini plexus was preserved. Dissection continued through the anterior prostate to the prostate apex. An incision was made between the prostate apex and the distal urethra. Finally, the dissected specimen was placed in a specimen bag. Pelvic lymphadenectomy was considered and performed in patients with a high risk of BCR.
- The vesicourethral anastomosis was started in the opposite direction to the traditional approach. From the 12 o’clock position of the bladder neck and urethra, two V-Loc sutures were placed as continuous sutures, one clockwise and the other counterclockwise. A new 18-Fr two-way Foley catheter was then inserted and filled with 150 cc of normal saline to check for leaks. After applying hemostatic material and positioning the drain, the peritoneal incision was closed using V-Loc suture material.
- 4. Statistical analysis
- All statistics were obtained using SPSS version 29 (IBM Corp.). Independent sample t-test, chi-square test were used for continuous and categorical variables, respectively. A p-value of 0.05 or less was considered statistically significant.
Methods
- Table 1 shows the demographic and preoperative characteristics of 69 patients who underwent RARP and rsRARP, respectively since March 2019. The mean age of the patients was 66.5±6.4 and 67.3±7.5 years in RARP and rs RARP, and the mean initial PSA level was 10.7±8.0 and 8.9±5.8 ng/mL in RARP and rs RARP, respectively. There was no difference in the D'Amico risk group and Gleason score at biopsy between the two groups.
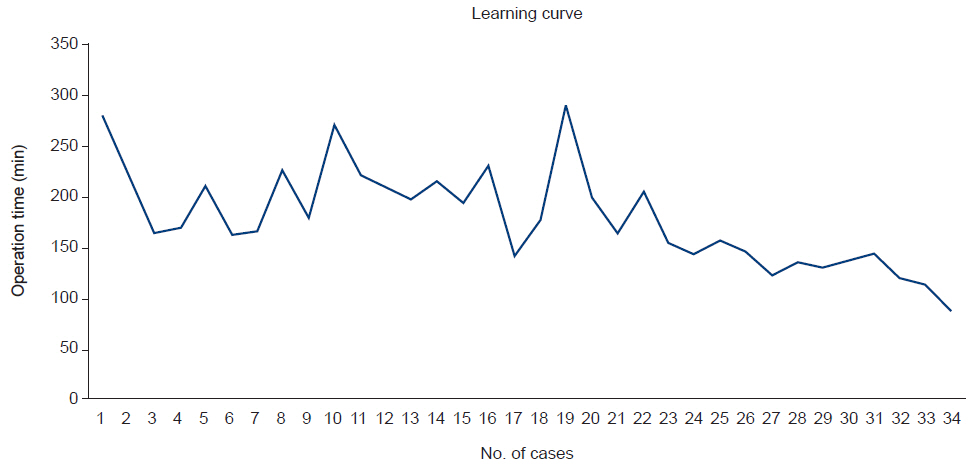
- Postoperative and pathologic features are shown in Table 2. Console time was 184.8±47.6 minutes and 178.9±48.3 minutes in RARP and rs RARP, respectively (p=0.752). The EBL was 397±267 and 364±305 (p=0.820), and two and seven patients were T3 or higher (p=0.067). There was no significant difference in Gleason score after surgery (p=0.408), and there were no patients with Clavien-Dindo grade 3 or higher (p=0.414). after surgery, urinary incontinence recovery at immediate, 1 month, 3 months, and 6 months (p<0.001, p=0.002, p=0.004, p=0.014) showed a significant difference between the two groups, but there were no differences at 12 months and PSM, potency, and postoperative BCR (p=0.083, p=0.348, p=0.581, p=0.299). Fig. 1 shows the change in the operating time from 279 to 87 minutes from the first case to the last case.
Results
- Prostatectomy has made remarkable progress over the past few decades due to innovations in anatomy, techniques, and devices. Walsh and Donker [8] presented the relationship between neurovascular bundles and potency, while Costello et al. [9] investigated neurovascular bundles and cavernosal nerves; studies have also been performed on the recovery of many nerves around the prostate, overall erectile function, and incontinence. The detrusor apron and Aphrodite veil have also been identified [10,11]. Segmentation of approaches, such as those in the intra-, inter-, and extrafascial planes, have also aided in functional preservation and recovery [12,13]. In addition, the advent of precision instrumentation, such as laparoscopes and robotics, offers oncologic and functional outcomes comparable to those of the past with increased surgical convenience.
- In 2010, Galfano et al. [5,14] presented a pure intrafascial approach called Retzius-sparing laparoscopic prostatectomy and reported on 200 surgical experiences. Lim et al. [6] demonstrated a statistically significant early recovery of continence through comparative studies using an anterior approach, and Dalela et al. [15] achieved the same with randomized controlled trial. The recovery of urinary continence after a follow-up of 12 months was also statistically significant in the meta-analysis by Checcucci et al. [16], whereas the PSM showed a low trend in the conventional technique. In addition, Nyarangi et al. [17] reported a surgical method that could be performed even in high-risk patients. Umari et al. [18], in a prospective comparative study of nearly 500 patients, showed that other indicators were similar and that quality of life was higher with faster recovery from urinary incontinence.
- Interesting studies on learning curves have also been reported, Olivero et al. [19] divided clinicians into two groups: experienced surgeons and “learning curve” surgeons with no prior experience in robotic radical prostatectomy but more than 50 experiences in first-assist or robotic lymph node dissection. They found rsRARP to be a safe and feasible technique even for those who are new to robotic surgery.
- The difference with this initial study is that a surgeon who had little experience with direct or indirect robotic prostatectomy, performed rsRARP surgery and compared it to the conventional method. The lack of experience with rsRARP is similar to that of many other hospitals. In addition, because rsRARP is a similar to the conventional method, it can be learned more quickly if the surgeon is familiar with RARP.
- The results of this study were also compared with the earlier study by Galfano and the study by Olivero [14,19]. These studies are considered to be the beginning of rsRARP, so they can be used as a comparison. The operation time and oncologic and functional outcomes of early cases showed similar results to Galfano's study. In Olivero's learning curve study [19], the rsRARP operators had the advantage of sharing the experience of more than 50 surgical assistants and experienced operators such as Galfano. Galfano was one of the pioneers of the rsRARP procedure and is therefore an expert in this technique. The average operative time for learning curve surgeons was 179 minutes for the first 248 patients [19]. The operative time shown in this study was similar and gradually decreased as the patients were operated. The decrease in operative time as the number of cases increases in Fig. 1 is similar to the graph of the first 200 cases by Galfano, showing that this surgical method has good reproducibility [14].
- Complications of Clavien-Dindo grade 3 or higher have not been reported, and it is believed that more surgical experience should be accumulated based on the incidence of complications reported by other authors. However, the absence of specific complications in these first 34 patients was a positive result in terms of the safety of the surgery. One patient who delayed conservative treatment experienced paralytic ileus and delayed catheter removal due to urine leakage on cystogram 1 week after surgery.
- Early recovery of urinary continence, which has been demonstrated in several studies, was also evident in this study because rsRARP preserved multiple structures anterior to the prostate. Complete dryness was observed in 74.5% of patients immediately after catheter removal on postoperative day 7 and in 88% at 12 months. This finding was similar to that of Lim et al. [6]. There are studies showing that there is no significant difference between the two surgical methods in the recovery of urinary continence at 12 months, and in this study the difference between the two groups decreased over time. However, the life satisfaction that urinary continence gives is not small [20].
- In the case of rsRARP, PSM appeared relatively frequently in the early cases, but did not appear in the later 12 cases. In addition, it did not appear in the anterior portion. The slightly higher PSM in rsRARP in this study may be due to insufficient surgical skill in the early stage.
- Since rsRARP separates the anterior part of the prostate in a similar way to the conventional basal and posterior parts, it can increase the possibility of PSM if there is cancer in the anterior part. Otherwise, surgical outcomes would be similar, as has been reported in recent studies showing similar results in PSM for each surgery [16]. Retzius-sparing surgery does not need to be performed if there is cancer in the anterior portion on preoperative examination. In addition, there is lymphatic tissue in the prostate anterior fat pad, and metastases are rarely found [21]. Therefore, prostatic fat pads should be carefully evaluated for lymph node metastasis prior to surgery and, if present, conventional surgical methods should be considered.
- There are several limitations to this initial experience with rsRARP. First, RARP was performed by an experienced surgeon and rsRARP was performed by a surgeon who was performing robotic prostatectomy for the first time, so there may be a difference in skill between the two procedures that could lead to errors in interpreting which method is better. A large randomized controlled trial performed in multiple hospitals and by multiple surgeons is needed before this approach becomes more established. Second, functional outcomes such as continence and potency were also subjectively assessed in this study, which may have influenced our results. A measurable functional comparison between rsRARP and RARP would be more objective and interesting.
- In conclusion, rsRARP is a highly reproducible procedure that even surgeons new to robotic prostate surgery can try. It is also a good surgical approach that shows oncologic results similar to the conventional approach with the advantage of early recovery of urinary incontinence.
Discussion
-
Conflicts of interest
No potential conflict of interest relevant to this article was reported.
-
Funding
None.
-
Author contributions
All the work was done by SHK.
Article information
Table 1.Demographic and preoperative features
Table 2.Postoperative and pathological features
- 1. Schuessler WW, Kavoussi LR, Clayman RV, et al. Laparoscopic radical prostatectomy: initial case report. J Urol 1992;147:246A.
- 2. Binder J, Kramer W. Robotically-assisted laparoscopic radical prostatectomy. BJU Int 2001;87:408–10.ArticlePubMedPDF
- 3. Abbou CC, Hoznek A, Salomon L, Lobontiu A, Saint F, Cicco A, et al. Remote laparoscopic radical prostatectomy carried out with a robot: report of a case. Prog Urol 2000;10:520–3.PubMed
- 4. Eastham JA, Scardino PT, Kattan MW. Predicting an optimal outcome after radical prostatectomy: the trifecta nomogram. J Urol 2008;179:2207–11.ArticlePubMedPMC
- 5. Galfano A, Ascione A, Grimaldi S, Petralia G, Strada E, Bocciardi AM. A new anatomic approach for robot-assisted laparoscopic prostatectomy: a feasibility study for completely intrafascial surgery. Eur Urol 2010;58:457–61.ArticlePubMed
- 6. Lim SK, Kim KH, Shin TY, Han WK, Chung BH, Hong SJ, et al. Retzius-sparing robot-assisted laparoscopic radical prostatectomy: combining the best of retropubic and perineal approaches. BJU Int 2014;114:236–44.ArticlePubMed
- 7. Menon M, Tewari A, Peabody J; VIP Team. Vattikuti Institute prostatectomy: technique. J Urol 2003;169:2289–92.ArticlePubMed
- 8. Walsh PC, Donker PJ. Impotence following radical prostatectomy: insight into etiology and prevention. J Urol 2002;167:1005–10.ArticlePubMed
- 9. Costello AJ, Brooks M, Cole OJ. Anatomical studies of the neurovascular bundle and cavernosal nerves. BJU Int 2004;94:1071–6.ArticlePubMed
- 10. Myers RP. Detrusor apron, associated vascular plexus, and avascular plane: relevance to radical retropubic prostatectomy: anatomic and surgical commentary. Urology 2002;59:472–9.Article
- 11. Walz J, Burnett AL, Costello AJ, Eastham JA, Graefen M, Guillonneau B, et al. A critical analysis of the current knowledge of surgical anatomy related to optimization of cancer control and preservation of continence and erection in candidates for radical prostatectomy. Eur Urol 2010;57:179–92.ArticlePubMed
- 12. Stolzenburg JU, Rabenalt R, Tannapfel A, Liatsikos EN. Intrafascial nerve-sparing endoscopic extraperitoneal radical prostatectomy. Urology 2006;67:17–21.Article
- 13. Budaus L, Isbarn H, Schlomm T, Heinzer H, Haese A, Steuber T, et al. Current technique of open intrafascial nerve-sparing retropubic prostatectomy. Eur Urol 2009;56:317–24.Article
- 14. Galfano A, Di Trapani D, Sozzi F, Strada E, Petralia G, Bramerio M, et al. Beyond the learning curve of the Retzius-sparing approach for robot-assisted laparoscopic radical prostatectomy: oncologic and functional results of the first 200 patients with ≥ 1 year of follow-up. Eur Urol 2013;64:974–80.Article
- 15. Dalela D, Jeong W, Prasad MA, Sood A, Abdollah F, Diaz M, et al. A pragmatic randomized controlled trial examining the impact of the Retzius-sparing approach on early urinary continence recovery after robot-assisted radical prostatectomy. Eur Urol 2017;72:677–85.Article
- 16. Checcucci E, Veccia A, Fiori C, Amparore D, Manfredi M, Di Dio M, et al. Retzius-sparing robot-assisted radical prostatectomy vs the standard approach: a systematic review and analysis of comparative outcomes. BJU Int 2020;125:8–16.ArticlePubMedPDF
- 17. Nyarangi-Dix JN, Gortz M, Gradinarov G, Hofer L, Schutz V, Gasch C, et al. Retzius-sparing robot-assisted laparoscopic radical prostatectomy: functional and early oncologic results in aggressive and locally advanced prostate cancer. BMC Urol 2019;19:113.ArticlePubMedPMCPDF
- 18. Umari P, Eden C, Cahill D, Rizzo M, Eden D, Sooriakumaran P. Retzius-sparing versus standard robot-assisted radical prostatectomy: a comparative prospective study of nearly 500 patients. J Urol 2021;205:780–90.ArticlePubMed
- 19. Olivero A, Galfano A, Piccinelli M, Secco S, Di Trapani D, Petralia G, et al. Retzius-sparing robotic radical prostatectomy for surgeons in the learning curve: a propensity score-matching analysis. Eur Urol Focus 2021;7:772–8.ArticlePubMed
- 20. Liss MA, Osann K, Canvasser N, Chu W, Chang A, Gan J, et al. Continence definition after radical prostatectomy using urinary quality of life: evaluation of patient reported validated questionnaires. J Urol 2010;183:1464–8.ArticlePubMed
- 21. Hansen J, Budaus L, Spethmann J, Schlomm T, Salomon G, Rink M, et al. Assessment of rates of lymph nodes and lymph node metastases in periprostatic fat pads in a consecutive cohort treated with retropubic radical prostatectomy. Urology 2012;80:877–82.ArticlePubMed
References
Figure & Data
References
Citations
Citations to this article as recorded by 


 KOSIN UNIVERSITY COLLEGE OF MEDICINE
KOSIN UNIVERSITY COLLEGE OF MEDICINE

 PubReader
PubReader ePub Link
ePub Link Cite
Cite