Articles
- Page Path
- HOME > Kosin Med J > Volume 33(3); 2018 > Article
-
Original Article
Comparative observational study of aminophylline with prophylactic and therapeutic uses for clinical outcomes in preterm infants - Mi Hye Bae, Na Rae Lee, Young Mi Han, Shin Yun Byun, Kyung Hee Park
-
Kosin Medical Journal 2018;33(3):380-385.
DOI: https://doi.org/10.7180/kmj.2018.33.3.380
Published online: December 31, 2018
Department of Pediatrics, Pusan National University Hospital Busan, Korea.
- Corresponding Author: Kyung Hee Park, Department of Pediatrics, Pusan National University Hospital, 179, Gudeok-ro, Seo-gu, Busan 49241, Korea. Tel: +82-51-240-7296, Fax: +82-51-248-6205, kuma2002@hanmail.net
• Received: March 27, 2018 • Revised: May 23, 2018 • Accepted: May 30, 2018
Copyright © 2018 Kosin University College of Medicine
Articles published in Kosin Medical Journal are open-access, distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
- 939 Views
- 4 Download
Abstract
-
Objectives
- Aminophylline has been used for prevention or treatment of apnea in preterm infants with idiopathic apnea of prematurity. The aim of this study was to assess the clinical usefulness of prophylactic in comparison with therapeutic aminophylline therapy.
-
Methods
- This retrospective observational study included infants born with a birth weight of < 2,500 g or at < 36 weeks of gestation. Infants born between August 2013 and July 2014 who received aminophylline therapy within 24 hr after birth were assigned to the prophylactic group, while infants born between August 2014 and July 2015 who received aminophylline therapy after obvious apnea were assigned to the therapeutic group. We compared clinical characteristics, including days of ventilator and oxygen therapy and bronchopulmonary dysplasia (BPD) between both groups.
-
Results
- Sixty—four patients and 25 infants were identified in the prophylactic and therapeutic groups, respectively. The mean gestational age and birth weight were 32.57 ± 1.96 weeks and 1765 ± 205 g, respectively, in the prophylactic group and 32.46 ± 1.82 weeks and 1770 ± 250 g, respectively, in the therapeutic group. No significant differences in clinical characteristics were found between the two groups. Similar clinical outcomes, including days of ventilator and oxygen therapy, intraventricular hemorrhage (IVH), periventricular leukomalacia, and BPD, were observed between the two groups.
-
Conclusions
- The present study showed that the prophylactic use of aminophylline does not improve the clinical outcomes, including BPD, IVH, and ventilator dependency as compared with therapeutic use. In other words, routine prophylactic use of aminophylline is unnecessary.
- Materials
- In accordance with our previous policy, aminophylline was administered prophylactically to infants born before July 2014 in our neonatal intensive care unit within 24 hr after birth. After this period we have been prescribing aminophylline only to infants who show obvious apnea. Apnea is defined as cessation of breathing for longer than 20 sec or for any duration if accompanied by cyanosis and bradycardia. Infants with major congenital anomalies, and other obvious problems resulting in apnea and death within 7 days of life were excluded. Apnea events were detected by attending physicians and nurses and documented using pulse oximetry monitors.
- On the basis of a different policy of aminophylline administration, infants were divided according prophylactic and therapeutic periods. Infants born with birth weights of < 2,500 g or at < 36 weeks of gestation were enrolled and assigned to two groups. Infants born between August 2013 and July 2014 who received aminophylline therapy within 24 hr after birth were assigned to the prophylactic group. Infants born between August 2014 and July 2015 who received aminophylline therapy after obvious apnea were assigned to the therapeutic group.
- Methods
- Demographic characteristics including gestational age and weight at birth, and sex were examined in both groups. For comparison of the outcome of aminophylline administration between prophylactic and therapeutic uses, the following parameters were analyzed: respiratory distress syndrome (RDS); patent ductus arteriosus (PDA, defined as the need for ibuprofen medication or surgical ligation), the duration of ventilator and oxygen therapy, intraventricular hemorrhage (IVH), periventricular leukomalacia (PVL), and BPD. Data were collected until death or discharge from the NICU.
- Standard protocol approval, registration, and patient consent
- Ethical approval for this study was granted by the institutional review board of our hospital (1801-013-163). The requirement for informed consent was waived because this study was conducted retrospectively.
- Statistical analysis
- Data were stored in a dedicated access database and verified for accuracy. Statistical analyses were performed with the SPSS 15.0 software by using raw scores. The analyses presented here focus on the comparisons between the two groups (prophylactic and therapeutic groups). Statistical comparison of the continuous and categorical variables was tested by means of t-test and chi-square test as appropriate for the data. In addition to univariate non-parametric statistical tests, the results of the t-test and chi-square tests were confirmed with the Mann-Whitney test and the Fisher's exact test. A p-value < 0.05 was regarded as statistically significant.
MATERIALS AND METHODS
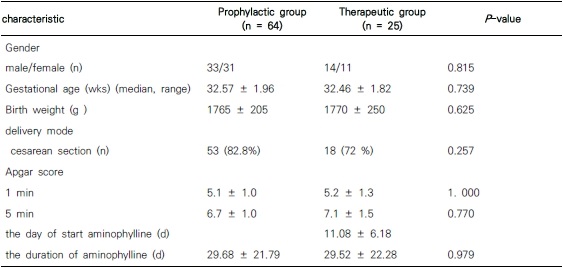
- Sixty—four patients and 25 infants were identified in the prophylactic and therapeutic groups respectively. Demographic findings showed no significant differences between the two groups. The mean gestational age was 32.57 ± 1.96 weeks in the prophylactic group, and 32.46 ± 1.82 weeks in the therapeutic group. The mean birth weights were 1765 ± 205 g and 1770 ± 250 g, respectively. The median time to initiation of aminophylline therapy was 11.08 ± 6.18 days in the therapeutic group (Table 1). The median duration of aminophylline therapy in the prophylactic and therapeutic groups were 29.68 ± 21.79 and 29.52 ± 22.28 days respectively (P = 0.979).
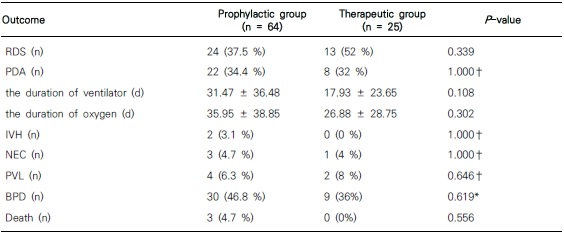
- The incidences of RDS and PDA were similar between the two groups. The durations of ventilator therapy in the prophylactic and therapeutic groups were 31.47 ± 36.48 and 17.93 ± 23.65 days respectively. The durations of oxygen therapy in the two groups were 35.95 ± 38.85 and 26.88 ± 28.75 days, respectively (Table 2). Although the therapeutic group seemed to have shorter durations of ventilator and oxygen therapies, the difference between the two groups was not statistically significant (P = 0.108 and P = 0.302, respectively). The outcomes such as IVH, PVL, NEC and BPD were similar between the two groups, indicating no significant difference between the two groups. Although three infants died in prophylactic group, there was no statistic significance. All these infants had less than 1,000 g of birth weight and died because of late onset sepsis.
RESULTS
- Apnea can lead to hypoxemia and bradycardia, particularly at very early gestational ages in preterm infants. Prolonged apnea presents clinical concerns about harmful effects on the development of the brain or dysfunction of the intestine and other organs. Bucher et al. reported that apnea and hypoxemia were associated with electroencephalographic abnormalities and maybe the causes of leukomalacia.5
- Methylxantines are most commonly used medications in apnea of preterm infants for more than 40 years.89 Although caffeine has now largely replaced aminophylline in western contries, aminophylline is mainly used in some contries including China.10 And there are also controversies about efficacy of caffeine compared to aminophylline.11
- In our NICU, infants born before July 2014 were given aminophylline prophylactically within 2 hr after birth. Recently, the effect of prophylactic use of aminophylline has been reported. Armanian et al. reported that prophylactic aminophylline was effective in reducing the apnea incidence in higher-risk neonates and that the median time of hospitalization was shorter in the aminophylline group than in the placebo group.7
- However, several studies reported no evidence of the benefit of using methylxanthines in preventing apnea in preterm infants. Henderson-Smart et al. reported that caffeine had no prophylactic effect on apnea of preterm infants.12 In addition, they reported that the results such as oxygen therapy period, amount of time needed for intubation, and incidence of chronic lung disease, cerebral palsy, major disabilities or death showed no significant differences between the prophylactic and placebo groups. Our NICU changed the policy of aminophylline administration from prophylactic use to therapeutic use, which means administration of aminophylline to infants showing obvious apnea. Therefore, we compared the outcomes of the prophylactic and therapeutic uses of aminophylline in infants born during two periods with different aminophylline administration policies with birth weight of < 2,500 g or < 36 weeks of gestational age.
- In our study, the mean gestational ages and birth weights were not significantly different between the prophylactic and therapeutic groups. Demographic findings also showed no significant differences between the two groups. Prophylactic use of aminophylline did not improve the clinical outcomes including RDS, BPD, NEC, IVH and ventilator dependency as compared with the therapeutic use. In other words, the prophylactic routine use of aminophylline is unnecessary because it brought no significant difference in clinical outcomes between the two groups.
- This study has important limitations. One is due to retrospective observational study and small number of infants included. Another is that the two groups included came from different periods, which might have affected the clinical outcomes. However, the policy in the care of preterm infants except the administration of aminophylline underwent no significant change. And the most important limitation is that we could not compare the serum concentrations of aminophylline between both groups.
- In conclusion, this study is in close agreement with the previous data of Henderson-Smart et al., which suggested that methylxanthine caused no clinical improvement in the outcome of apnea in preterm infants.12 In addition, therapeutic use of aminophylline might be adequate for infants who show obvious apnea. In our knowledge, this is the first study to compare the outcome of the prophylactic and therapeutic uses of aminophylline therapy in Korea. Further studies with adequate sample size and prospective studies are needed to investigate the effectiveness and clinical outcomes of the prophylactic and therapeutic uses of aminophylline.
DISCUSSION
Acknowledgments
Acknowledgement
- 1. Finer NN, Higgins R, Kattwinkel J, Martin RJ. Summary proceedings from the apnea-of-prematurity group. Pediatrics 2006;117:S47–S51.ArticlePubMed
- 2. Committee on Fetus and Newborn, American Academy of Pediatrics. Apnea, sudden infant death syndrome, and home monitoring. Pediatrics 2003;111:914–917.ArticlePubMedPDF
- 3. Henderson-Smart DJ, Steer P. Methylxanthine treatment for apnea in preterm infants. Cochrane Database Syst Rev 2001;8:CD000140.Article
- 4. Henderson-Smart DJ, Steer PA. Caffeine versus theophylline for apnea in preterm infants. Cochrane Database Syst Rev 2010;20:CD000273.Article
- 5. Bucher HU, Duc G. Does caffeine prevent hypoxaemic episodes in premature infants? A randomized controlled trial. Eur J Pediatr 1988;147:288–291.ArticlePubMed
- 6. Levitt GA, Mushin A, Bellman S, Harvey DR. Outcome of preterm infants who suffered neonatal apnoeic attacks. Early Hum Dev 1988;16:235–243.ArticlePubMed
- 7. Armanian AM, Badiee Z, Afghari R, Salehimehr N, Hassanzade A, Sheikhzadeh S, et al. Prophylactic aminophylline for prevention of apnea at higher-risk preterm neonates. Iran Red Crescent Med J 2014;16:e12559.ArticlePubMedPMC
- 8. Kuzemko JA, Paala J. Apnoeic attacks in the newborn treated with aminophylline. Arch Dis Child 1973;48:404–406.ArticlePubMedPMC
- 9. Aranda JV, Gorman W, Bergsteinsson H, Gunn T. Efficacy of caffeine in treatement of apnea in the low-birth-weight infant. J Pediatr 1977;90:467–472.ArticlePubMed
- 10. Chen C, Shu XX, Yang XY, Shi J, Tang J, Mu DZ. Current research status of durg therapy for apnea of prematurity. Zhongguo Dang Dai Er Ke Za Zhi 2016;18:806–811.PubMedPMC
- 11. Abdel-Hady H, Nasef N, Shabaan AE, Nour I. Caffeine therapy in preterm infants. World J Clin Pediatr 2015;8:81–93.Article
- 12. Henderson-Smart DJ, De Paoli AG. Prophylactic methylxanthine for prevention of apnoea in preterm infants. Cochrane Database Syst Rev 2010;8:CD000432.Article
References
Figure & Data
References
Citations
Citations to this article as recorded by 


 KOSIN UNIVERSITY COLLEGE OF MEDICINE
KOSIN UNIVERSITY COLLEGE OF MEDICINE
 PubReader
PubReader Cite
Cite
