Emergency rescue stent grafting for a ruptured degenerated graft that bypassed coarctation of the aorta: a case report
Article information
Abstract
A 33-year-old man who had undergone bypass from the distal aortic arch to the proximal descending thoracic aorta with a Dacron graft to treat coarctation of the aorta 20 years prior presented to the emergency department with massive hemoptysis. He was diagnosed with a graft-to-bronchial fistula. After thoracic endovascular aneurysm repair through the coarctation, aortic replacement was performed 3 weeks later. Therefore, emergency-rescue thoracic endovascular aneurysm repair can be considered for preventing aortic rupture.
Introduction
In the literature, most late complications of Dacron grafts are anastomotic pseudoaneurysm, fistula, graft thrombosis, graft infection, or non-anastomotic aneurysmal change or rupture. Some reports on endovascular repair of Dacron graft dilatation with a subsequent anastomotic false aneurysm after post-coarctation aortic repair demonstrated the feasibility of endovascular treatment in selected candidates because it is not appropriate for all graft failure cases or for cases that require long-term follow-up for graft stability [1]. In this case, first of all we performed thoracic endovascular aneurysm repair (TEVAR) successfully to stabilize the patient’s vital signs due to the risks associated with emergent aortic replacement.
Case
Ethical statements: This study was approved by the Institutional Ethics Committee of Daejeon Eulji University Hospital (EMC 2021-08-004). Informed consent was obtained from the patient.
A 33-year-old male patient was admitted with hemoptysis that measured about one liter. A bypass from the distal arch to the proximal descending thoracic aorta with a Dacron graft was achieved to treat coarctation of the aorta that had occurred 20 years prior. Additional bypass grafting from the right axillary to the femoral artery was performed 5 years after the initial procedure because of deterioration of coarctation. Hemoptysis originated from a graft-to-bronchial fistula, identified at a degenerative aneurysm of the Dacron graft. The diameter of the severely twisted graft on computed tomography (CT) scans was 20 mm (Fig. 1A). Although no interval change had been detected on scans obtained at 8 and 12 years, a CT scan in the emergency department revealed a diameter increase to 38 mm (Fig. 1B). TEVAR through coarctation and simultaneous extra-anatomic bypass grafting from the ascending to descending thoracic aorta were planned.
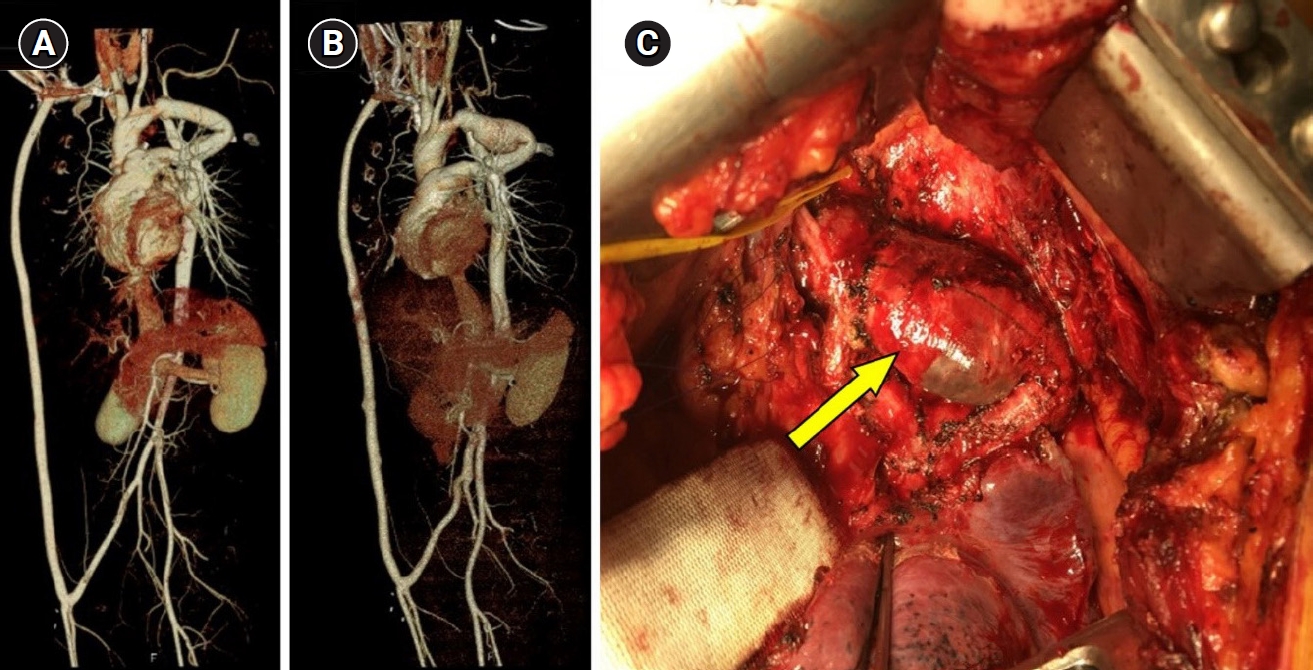
Computed tomography scans from 8 years ago (A) and at presentation (B). Twisted graft with aneurysmal change at the rupture spot (arrow in C).
However, he presented at our hospital one day prior to admission for TEVAR due to massive hemoptysis. His medical condition was unstable. A follow-up CT scan showed increased graft size to 41 mm. We decided to perform an emergent TEVAR for coarctation of the aorta and aortic replacement when the patient’s vital signs stabilized.
A 10-mm balloon angioplasty prior to TEVAR allowed the TEVAR catheter to pass the coarctation. After TEVAR using a Medtronic Valiant thoracic stent graft (22 mm in diameter, 150 mm in length; Medtronic Vascular, Santa Rosa, CA, USA) (Fig. 2A), hemoptysis was resolved. The coarctation, however, was not sufficiently relieved, and the degree of dependence on the axillofemoral bypass graft increased. After 3 weeks of recovery from pneumonia and TEVAR, the final aortic replacement was implemented after the ruptured spot on the crisp graft was located (Fig. 1C, arrow). The aorta was replaced with a 22 mm Hemashield platinum woven double velour straight graft (Maquet Getinge Group, Rastatt, Germany) (Fig. 2B). Preoperative blood pressure was 131/63 mmHg in the right radial artery and 86/52 mmHg in the descending thoracic aorta, and the postoperative values were 122/70 mmHg and 110/69 mmHg, respectively.
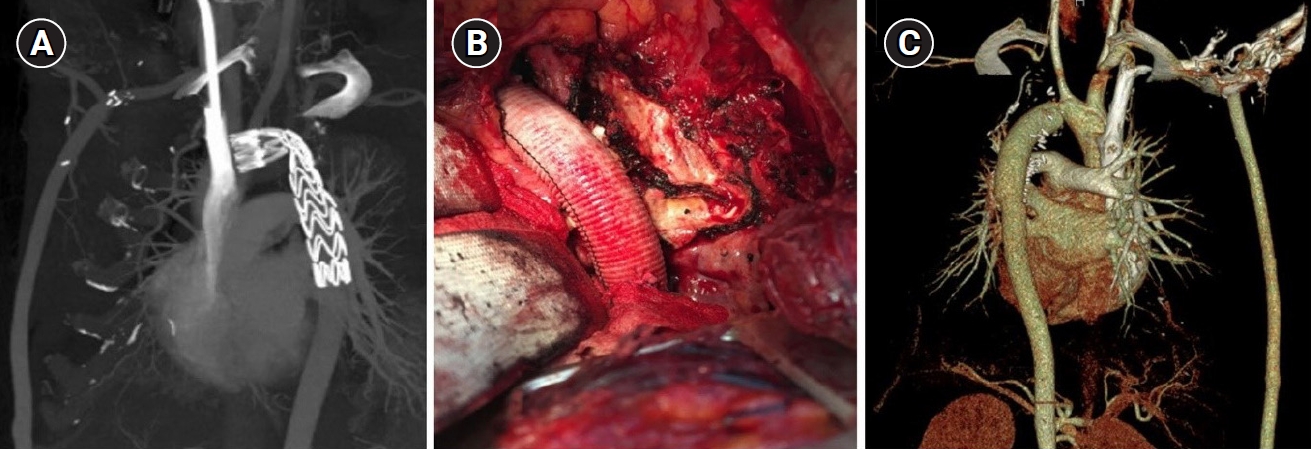
Computed tomography (CT) scan after thoracic endovascular aneurysm repair, without any definite endoleak (A). The new Dacron graft in the operative findings (B) and a postoperative CT scan (C).
The patient was discharged on postoperative day 10 without complications. Postoperative, 6-month follow-up CT scan showed no abnormality (Fig. 2C).
Discussion
This case report provides two significant insights: degenerative rupture of a Dacron graft and TEVAR as a therapeutic option for aortic rupture.
Previous reports indicated that most late complications of Dacron grafts are anastomotic pseudoaneurysm, fistula, graft thrombosis, graft infection, or non-anastomotic aneurysmal change or rupture [1]. Complications associated with woven Dacron have been reported [2]. For this patient, the graft was in a twisted position for a long time, and the increase of afterload in the graft proximal to twisting resulted in gradual aneurysmal changes and, finally, graft rupture.
Previous reports on endovascular repair of Dacron graft dilatation with a subsequent anastomotic false aneurysm after post-coarctation aortic repair demonstrated the feasibility of endovascular treatment in select candidates; however, this approach is not appropriate for all graft failure cases or for cases that require long-term follow-up for graft stability [2].
In the present case, TEVAR was implemented to stabilize the patient’s vital signs [3] due to the risks associated with emergent aortic replacement [4].
Recent reports have indicated that systolic pressure gradients were reduced significantly to 4±6 mmHg after TEVAR [5]. In the present case, however, the systolic pressure gradient was 45 mmHg (131 mmHg vs. 86 mmHg), and the internal diameter was less than 10 mm. Therefore, the next aortic replacement was planned based on patient age, risk of progressive cardiac afterload or cerebral hypertension, and delayed complications of TEVAR.
Notes
Conflicts of interest
No potential conflict of interest relevant to this article was reported.
Funding
None.
Author contributions
Conceptualization: JHC, MSC, HL. Data curation: JHC, MSC, HL. Formal analysis: JHC, MSC, HL. Methodology: JHC, HL. Project administration: JHC, MSC, HL. Visualization: MSC. Writing-original draft: JHC, MSC, HL. Writing-review & editing: JHC, HL. Approval of final manuscript: JHC, MSC, HL.
