Perioperative cutaneous complications in an elderly patient due to inappropriate use of a forced-air warming device and underbody blanket: a case report
Article information
Abstract
Forced-air warming is commonly utilized to prevent perioperative hypothermia. Underbody warming blankets are often employed to secure a larger area for patient warming. While forced-air warming systems are generally regarded as safe, improper usage poses a risk of cutaneous complications. Additionally, the influence of underbody blankets on cutaneous complications remains uncertain. We present a case of cutaneous complications resulting from the improper utilization of a forced-air warming device and an underbody blanket. A 79-year-old man presented to the hospital for robotic proctectomy under general anesthesia. The surgery lasted for 7 hours, and the forced-air warming device with underbody blanket operated continuously for 5 hours intraoperatively. The surgery was completed without any incidents. However, first-degree burns on the patient’s back, along with superficial decubitus ulcers on his right scapula, were observed after surgery. To prevent cutaneous complications, clinicians must adhere to the manufacturer's guidelines when utilizing a forced-air warming system. Compared to overbody blankets, underbody blankets have limitations in monitoring cutaneous responses. Ensuring patient safety requires selecting an appropriate blanket for scheduled operations.
Introduction
Perioperative hypothermia is a common issue, which can lead to various complications such as cardiac abnormalities, impaired wound healing, increased surgical site infections, and coagulopathies [1]. To prevent perioperative hypothermia, a forced-air warming (FAW) system has been commonly utilized with the attachment of a warming blanket. Warming blankets are often used by covering patients, but they are sometimes placed underneath patients to secure sufficient skin warming, especially in surgeries with a wide surgical area such as abdominal surgery [2]. However, the effect of the underbody blanket on the patient's cutaneous complications is not clear. Additionally, although the FAW system is widely used as a safe device, there is a risk of burns or pressure ulcers, especially when used improperly [3,4]. We present a case of pressure ulcers and low-temperature burns in an elderly patient who underwent prolonged surgery under general anesthesia with an underbody warming blanket. Although cutaneous complications caused by the misuse of the FAW system are not novel discoveries, we consider our case report valuable due to its educational significance for other clinicians in terms of the proper utilization of the FAW system [5].
Case
Ethical statements: This study was exempted from review by the Institutional Review Board of Inje University Busan Paik Hospital (IRB No: 2023-01-038). Informed consent was waived due to the retrospective study.
A 79-year-old man presented to the hospital for robotic proctectomy under general anesthesia. He had a history of rectal cancer and had undergone transarterial chemoembolization treatment for hepatic cellular carcinoma but was otherwise healthy. He was premedicated intramuscularly with 0.2 mg glycopyrrolate and 20 mg famotidine. Before he entered the operating room, an FAW blanket (Bair Hugger, Model 63500; Arizant Healthcare, Inc.) was placed on the surgical bed. After he lay on the surgical bed, the Bair Hugger warming device (Model 505; Arizant Healthcare, Inc.) was attached to the blanket to provide him warmth. In addition to the FAW system, a heating circuit system (Mega Acer kit; ACE Medical) was employed to maintain the patient’s body temperature. Anesthesia was induced with propofol, lidocaine, and remifentanil, and rocuronium was injected to facilitate endotracheal tube insertion. Anesthesia was maintained with sevoflurane administration and continuous remifentanil and rocuronium infusion. For more precise monitoring of the patient's condition intraoperatively, a central venous catheter was inserted into the right internal jugular vein and an arterial catheter into the left radial artery. The patient’s body temperature was measured using a Bair Hugger temperature monitoring sensor (Model 36000; Arizant Healthcare, Inc.) attached to his forehead. Thirty minutes after the surgery began, the patient’s body temperature measured 36.3 °C (Fig. 1). The surgery lasted for 7 hours, and the patient maintained a lithotomy position for 1 hour, a lithotomy-Trendelenburg position (Fig. 2) for 5 hours and 30 minutes, and a supine position for 30 minutes. No complications occurred intraoperatively, and the patient’s vital signs were within normal limits. The FAW device operated at a high temperature (43.0 °C), and both the FAW device and heating circuit system were turned off when his body temperature reached 37.8 °C, 5 hours after the surgery started. After surgery, his body temperature was 37.7 °C. After tracheal extubation, he was transferred to the surgical intensive care unit. During the examination of the patient’s skin in the surgical intensive care unit, his back skin was generally reddish. Large skin erosions at 10×5 and 5×8 cm on the right scapula (Fig. 3) and reddish linear skin lesions around the shoulder were observed (Fig. 4). He complained of an itching sensation on his back. The hospital dermatologist diagnosed the skin lesions as superficial decubitus ulcers and first-degree burns, which appeared to have resulted from prolonged exposure to warm air convected by underbody blanket. His skin was treated symptomatically, and he was transferred to a general ward on postoperative day 2. On postoperative day 12, he was discharged from the hospital without any observed complications.
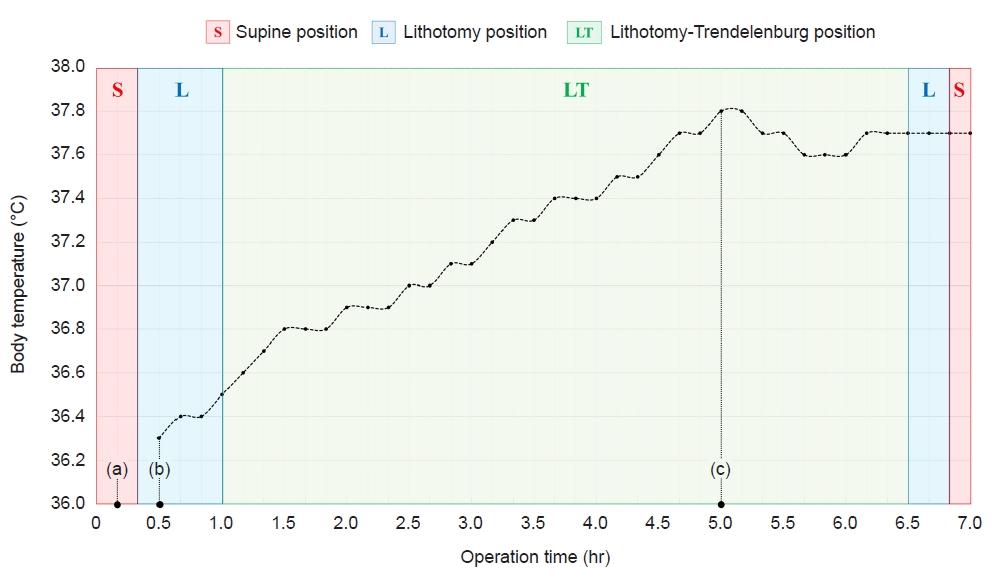
Changes in body temperature and surgical position. (a) Start of induction of general anesthesia. (b) Start measuring body temperature. (c) Turning off the forced-air warming system. The changes in the patient's position during surgery are differentiated by boxes of different colors.

Lithotomy-Trendelenburg position. Bilateral shoulder supports (black arrowheads) were used so that the patient would not slip from the bed intraoperatively.

Skin erosions on the right scapula. The areas of erosion measured 10×5 and 5×8 cm. The image has been altered to obscure any personal identifying information of the patient.
Discussion
The FAW system maintains patients’ body temperature by transferring heat through warm air convection and preventing heat loss from the areas covered by the blanket [6]. Due to this mechanism, the larger the area covered by the blanket, the greater the efficiency of the FAW system [7]. Along with surgical draping, the underbody blanket secures a larger body surface and enables sufficient warm air convection over the patient’s body [2]. However, periodically assessing the patient's skin in contact with the underbody blanket during surgery poses a challenge. Additionally, the underbody blanket can experience limitations in expansion due to manipulation of the surgical bed, such as tilting, which can result in partial compression of the blanket against the patient. The restrictions in blanket expansion can force air into smaller areas, potentially increasing the risk of burns [8]. These facts suggest that the utilization of underbody blankets may impact the occurrence of perioperative cutaneous complications in patients. However, due to the lack of research on the relationship between underbody blankets and cutaneous complications, it is difficult to determine whether the utilization of underbody blankets increases the occurrence of perioperative cutaneous complications.
There are two hypotheses regarding the mechanism behind the development of skin lesions in our patient. The first hypothesis attributes the development of the pressure ulcer to a cascade of events initiated by a mild burn from prolonged heat exposure caused by the underbody blanket, subsequently compounded by pressure due to the surgical position. The epidermis, compromised by the mild burn, would have become vulnerable to pressure and friction, thus making the development of pressure ulcers more likely. The second hypothesis supposes that hyperthermia, independent of the occurrence of a burn, contributed to the development of the pressure ulcer. Pressure ulcers occur due to tissue ischemia and necrosis resulting from sustained and excessive external pressure [9]. As the body temperature increases, the metabolic rate and oxygen consumption of the tissue also increase [10]. The elevated metabolic rate and oxygen consumption of the tissue would worsen tissue necrosis, consequently leading to the development of pressure ulcers.
Since burns related to the utilization of the FAW system are rare when adhering to the manufacturer's guidelines, the majority of burn cases resulting from the use of the FAW system are a consequence of its misuse [4]. The most common misuse of the FAW system is “hosing,” which involves using the FAW device without a blanket and can result in burns to patients, even with short-term use [4,11]. Brauer et al. [12] reported severe cutaneous complications in a patient using an underbody blanket, likely resulting from warming the lower extremities during aortic cross-clamping. This practice is contraindicated according to the manufacturer’s guidelines. Although we used the FAW device with a blanket in non-cardiac surgery in this case, our adherence to the manufacturer's guidelines was deficient in several aspects.
Firstly, we did not adjust the air temperature or stop warming when the patient's body temperature was normalized, as outlined in the manufacturer's guidelines. The NICE (National Institute for Health and Care Excellence) guidelines recommend maintaining the patient's body temperature between 36.5 and 37.5 °C [13]. Adjusting the air temperature not only prevents hyperthermia but also reduces the rate of sweating for patients, leading to increased thermal comfort and satisfaction [14]. However, we did not focus on the patient and were negligent in monitoring vital signs. As a result, we only realized later on that the patient's body temperature had risen too high. We should have been monitoring the patient's body temperature regularly and considering adjusting the air temperature or halting the operation of the FAW system when the patient's body temperature was within the normal range.
We also failed to properly monitor our patient's cutaneous response, which is crucial for preventing complications. The manufacturer's guidelines recommend checking every 10 to 20 minutes when the FAW system is used for non-communicative individuals. It was challenging to closely examine the cutaneous response of a patient surrounded by an underbody blanket and surgical draping during surgery. Despite the difficulty, we acknowledge our lapse in monitoring. With more vigilant observation, we could have identified cutaneous complications earlier, enabling faster intervention.
Finally, the underbody blanket we utilized, Bair Hugger (Model 63500), is recommended for supine, prone, and lateral positions, but not for steep Trendelenburg position in robot-assisted surgery. While the product manual does not explicitly prohibit the use in the Trendelenburg position, there is currently no research indicating the safety of using it in this position. Therefore, opting for a blanket recommended for use even in the Trendelenburg position, such as an overbody blanket, appears to be safer for the patient.
To prevent cutaneous complications, clinicians must utilize the FAW system following the manufacturer's guidelines. During surgery, anesthesiologists should continuously monitor vital signs and periodically evaluate patients’ cutaneous responses to the utilization of the FAW system. While the underbody blanket effectively prevents hypothermia, there is a potential for it to have a negative impact on the occurrence of cutaneous complications. To ensure patient safety, an appropriate blanket should be chosen for the scheduled surgery.
Notes
Conflicts of interest
No potential conflict of interest relevant to this article was reported.
Funding
None.
Author contributions
Conceptualization: SK. Data curation: MK, SJL. Investigation: BC, GL. Methodology: SK, MK. Project administration: SK, MK. Resources: BC, GL. Supervision: MK. Validation: MK, SJL. Visualization: GL. Writing – original draft: SJL, BC. Writing – review & editing: SK, MK.

