Remote health monitoring services in nursing homes
Article information
Abstract
Aged people are challenged by serious complications from chronic diseases, such as mood disorder, diabetes, heart disease, and infectious diseases, which are also the most common causes of death in older people. Therefore, elderly care facilities are more important than ever. The most common causes of death in elderly care facilities were reported to be diabetes, cardiovascular disease, and pneumonia. Recently, the coronavirus disease 2019 (COVID-19) pandemic have a great impact on blind spots of safety where aged people were isolated from society. Elderly care facilities were one of the blind spots in the midst of the pandemic, where major casualties were reported from COVID-19 complications because most people had one or two mortality risk factors, such as diabetes or cardiovascular disease. Therefore, medical governance of public health center and hospital, and elderly care facility is becoming important issue of priority. Thus, remote health monitoring service by the Internet of Medical Things (IoMT) sensors is more important than ever. Recently, technological breakthroughs have enabled healthcare professionals to have easy access to patients in medical blind spots through the use of IoT sensors. These sensors can detect medically urgent situations in a timely fashion and make medical decisions for aged people in elderly care facilities. Real-time electrocardiogram and blood sugar monitoring sensors are approved by the medical insurance service. Real-time monitoring services in medical blind spots, such as elderly care facilities, has been suggested. Heart rhythm monitoring could play a role in detecting early cardiovascular disease events and monitoring blood glucose levels in the management of chronic diseases, such as diabetes, in aged people in elderly care facilities. This review presents the potential usefulness of remote monitoring with IoMT sensors in medical blind spots and clinical suggestions for applications.
Introduction
The entering of a super-aged society and health-related quality of life is becoming more important than ever [1]. The Ministry of Health and Welfare reported a growing super-aged society from 15.7% to 17.3% of the proportion of the population aged 65 and above (Fig. 1). With the rapid entry into a super-aged society, growing socioeconomic problems, which cause sharp increases in chronic disease-related complications, have been reported [1].
The number of aged patients with severe illness or death from coronavirus disease 2019 (COVID-19) infections in Korea is significantly high compared to younger patients (Fig. 2) [2]. The recent COVID-19 pandemic caused serious problems in residents in elderly care facilities in Korea, including nursing homes and elderly daycare centers.
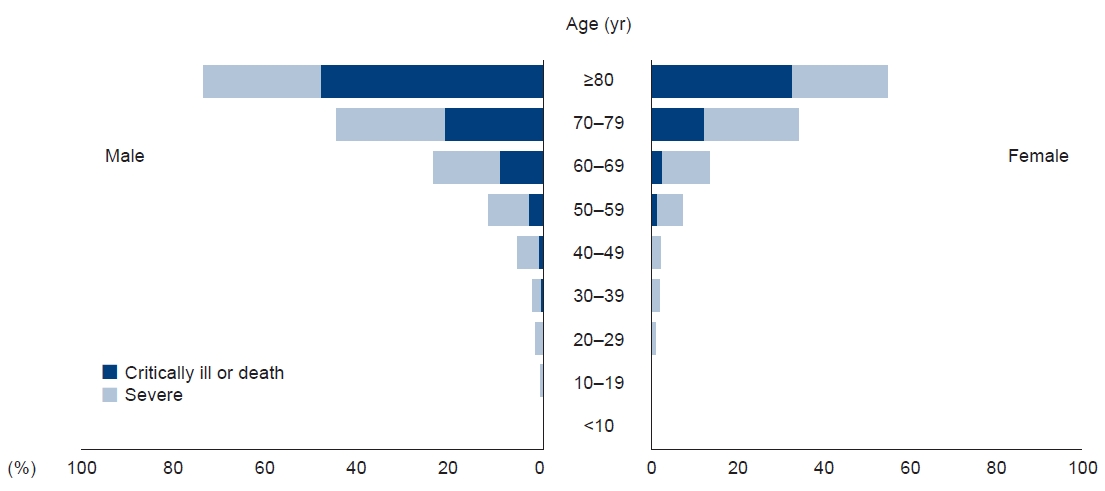
Age and sex relationships with clinical severity during hospitalization or isolation from coronavirus disease 2019 (COVID-19).
1. Increasing issue of medical blind spots: elderly care facilities
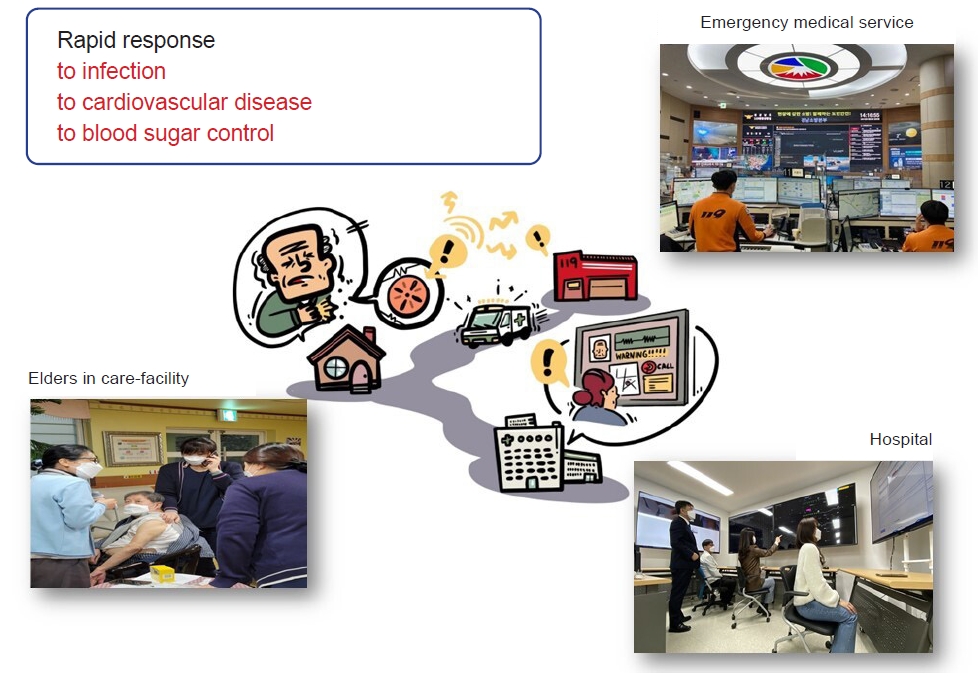
The main users of elderly care facilities are aged people with underlying diseases, and the rate of death from COVID-19 infections is very high. Among the total cumulative deaths from COVID-19 in Korea, the number of deaths due to infections in elderly care facilities is high [3,4]. Another outbreak of a COVID-19 strain variant is inevitable, and medical solutions to prepare for infections in elderly care facilities should be considered from a public governance perspective.
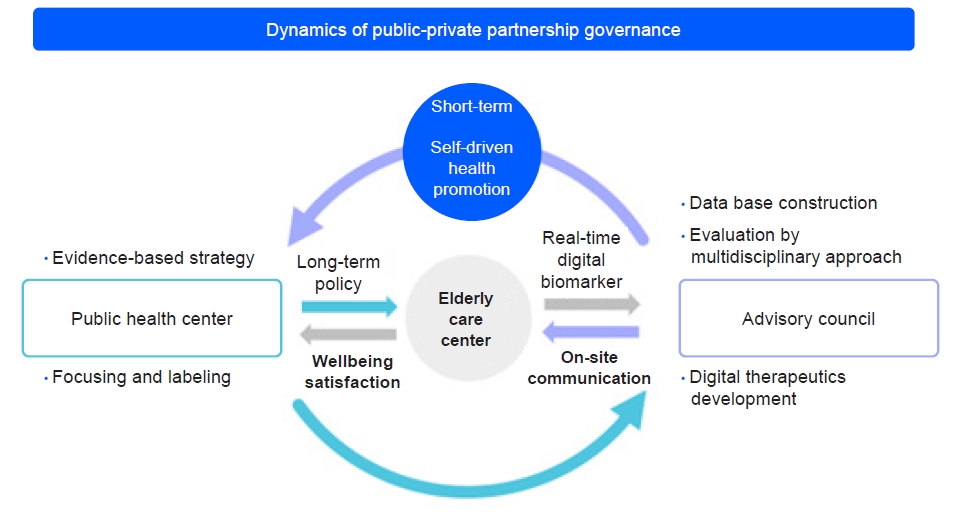
2. Governance of public health, private health, and care facilities
The main reason for such great casualties in elderly care facilities in the midst of the pandemic was the lack of communication between hospital professionals and medical staff in elderly care facilities. The medical staff of quarantined care facilities were isolated not only spatially but also medically, so no guidance from secondary advisory consultants could be provided [5]. Therefore, the medical governance of public health centers, hospitals, and elderly care facilities is becoming an important issue (Fig. 3).
3. Alternative solution for communication between care facilities and general hospitals
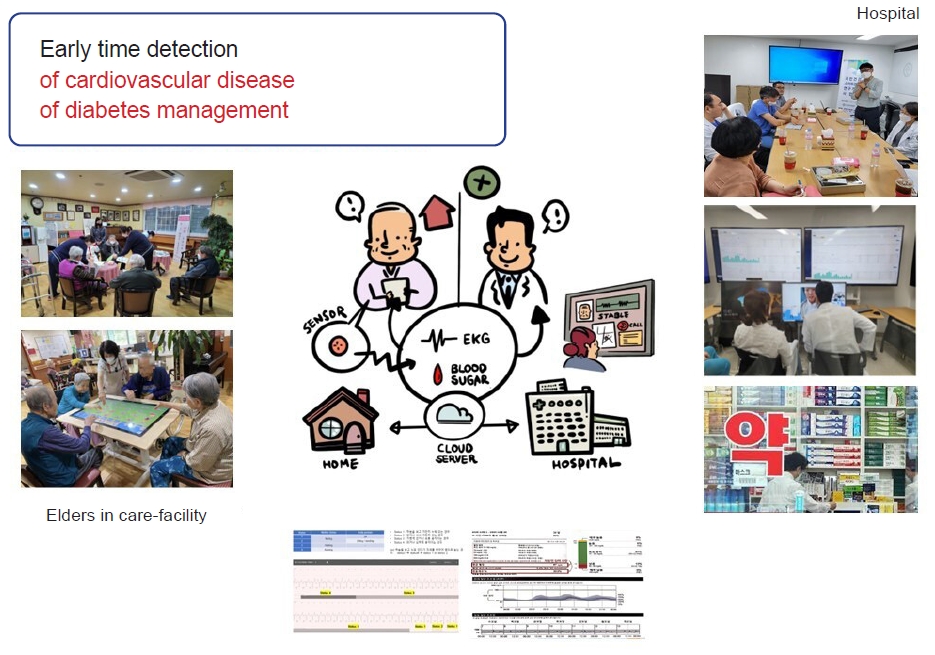
Based on the above situation, healthcare professionals are greatly challenged to develop new healthcare services to overcome the increasing service burden. The recent development of information, communications, technology technologies has enabled healthcare providers to investigate how to enhance healthcare services in response to the aging population issue [6-8]. Based on smart healthcare and recent innovations, home care technology, such as remote-monitoring services, is becoming a new complementary solution to transform the healthcare industry (Fig. 4).
4. Recent breakthrough in remote health monitoring services
Internet of Medical Things (IoMT)-based remote health monitoring services have been demonstrated as a challenging modality for communicating with elderly care facilities [9,10]. IoMT-based devices, such as real-time electrocardiogram (EKG) monitoring and continuous glucose monitoring sensors, gather digital data using a cloud server [11-14]. The visualization of digital biomarkers from EKG and blood glucose monitoring with a phone gateway helps patients achieve motivation for self-driven lifestyle modifications based on biofeedback from digital data from IoMT sensors (Fig. 5).
Clinically application of IoMT devices in elderly care facilities
1. Early detection of subclinical cardiovascular and infectious diseases
Real-time EKG monitoring is clinically useful in the detection of abnormal heart rhythms, such as arrhythmias and coronary diseases [15]. If the real-time EKG monitoring of high-risk patients in care facilities were possible, abnormalities could be detected early and proper medical precautions could be taken. As mentioned above, reports have demonstrated that the real-time EKG monitoring of higher-risk patients with cardiovascular diseases achieved early diagnoses and timely treatment [16]. Therefore, this medical evidence should be extended to applications in care facilities.
In the field of home care diagnostics, the use of artificial intelligence (AI)-powered diagnostic technologies, such as portable X-ray and ultrasound imaging, for patients in inaccessible areas at home or isolated facilities, is challenging [17-20]. Therefore, AI-powered digital imaging technology connected to real-time EKG monitoring is specifically promising for early detection, and intelligent platforms can assist in decision support and help recognize acute conditions in patients with fatal infectious diseases like COVID-19.
2. Evaluation and management of chronic diseases like diabetes
Well-thought-out blood glucose self-monitoring can monitor a patient's glycemic status [21-23]. IoMT sensors can easily visualize and continuously record blood glucose monitoring data. This can be done mainly by a nurse or medical assistant in care facilities. These data are registered in a cloud server and reviewed by medical professionals, as well as care providers in care facilities, with the consent of the patient (Fig. 6). The patient and caregiver can use the analysis by advisory consultants for timely decision-support messages about the management of chronic diseases, i.e., lifestyle modification or supporting medication [24,25]. This collaboration between care facilities and hospitals may facilitate customized care services to improve the quality of life of patients with chronic diseases.
3. Digital literacy of aged people and evaluation of care services
IoMT-based healthcare services may improve the quality of life for people in care facilities. However, the main obstacle to applying IoMT technology is digital illiteracy. Caregivers must consider the role of medical assistants and nurses in care facilities. Their experiences and motivation for aged people with chronic diseases are essential for achieving remote health monitoring services in care facilities. Therefore, it is vital to establish the digital phenotyping of aged people in regard to simplicity and functionality. Aged people could suffer from a lack of digital experiences, resulting in the impairment of cognitive function [26,27].
Conclusion
IoMT-based smart healthcare services, especially remote health monitoring services, have become more acceptable. These technologies may provide useful opportunities for preparing safe medical solutions in the midst of the COVID-19 pandemic using real-time patient monitoring resources and services. Real-time EKG monitoring services are used to make early diagnoses of patients with infectious and cardiovascular diseases. Continuous glucose monitoring services have significant potential to achieve the modification of chronic diseases, such as diabetes. Therefore, IoMT sensors may be used to collect useful data from care facilities so that rapid advisory consulting and timely decision-making could be possible for elderly patients.
Notes
Conflicts of interest
This project was supported by LEENO industrial company. Except for that, no potential conflict of interest relevant to this article was reported.
Funding
This work was supported by the Korea Health Industry Development Institute (KHIDI 20210048001).
Author contributions
Conceptualization: CO. Data curation: SI. Formal analysis: SK, SI. Funding acquisition: CO. Investigation: HK. Methodology: HYL, YC. Project administration: CO. Software: CO. Supervision: LS. Validation: YC. Visualization: YP. Writing - original draft: JK. Writing - review & editing: CO, JK.