A Case of Malignant Lymphoma Misdiagnosed as Acute Tonsillitis with Subsequent Lymphadenitis
Article information
Abstract
A 56-year-old female presented with clinical features of acute tonsillitis with subsequent cervical lymphadenitis. After taking empirical antibiotics for 1 week, the acute infection symptoms and signs were resolved. However, an asymmetric enlargement of the left palatine tonsil with ipsilateral neck swelling remained. Subsequent tonsillectomy and lymph node excisional biopsy were performed due to the possibility of malignancy. The patient was eventually diagnosed as malignant lymphoma according to pathological confirmation. We demonstrate the diagnostic challenges in such a rare case and emphasize the importance of differentiating malignant lymphoma from an atypically presenting acute infectious disease.
Lymphoma comprises 12–15% of head and neck cancer cases, and about 25% of head and neck lymphomas occur in the extranodal area.1 About half of extranodal head and neck lymphomas occupy Waldeyer ring, most commonly in the palatine tonsils, followed by the nasopharynx, oropharynx, thyroid, salivary glands, and paranasal sinuses.2 Diffuse large B-cell lymphoma (DLBCL) comprises 65–85% of the histological types and usually presents as painless cervical lymph node enlargement without accompanying B symptoms such as fever, night sweat, or weight loss.3 Other systemic symptoms are observed in < 10% of stage I or II disease and 30–40% of stage III or IV disease.4
Unilateral tonsillar enlargement can be seen in cases of recurrent tonsillitis, chronic tuberculosis, innate tonsillar asymmetry, and tumors in the tonsils or parapharyngeal spaces.5 Therefore, after ruling out benign conditions of unilateral tonsillar enlargement, there should be suspicious of a malignant conditions, and a diagnostic tonsillectomy is recommended, especially in an adult.6
The common symptoms of acute tonsillitis are sore throat, fever, chills, and sometimes swallowing difficulty. Reactive cervical lymph node enlargement or lymphadenitis may also occur. If lymph nodes are tender and fever is present It would be a benign inflammatory condition rather than a malignancy, and antibiotics with conservative treatment would be administered.7 However, we experienced a rare adult female patient who initially presented with acute tonsillitis and cervical lymphadenitis but who was finally diagnosed with DLBCL. We report the case to emphasize the importance of a careful evaluation and close follow-up of similar cases.
CASE
A 56-year-old woman who had visited a primary clinic for sore throat and fever for 1 week was referred to our tertiary hospital due to the lack of a response to medications including oral ampicillin under the diagnosis of acute tonsillitis. She had no history of recurrent acute tonsillitis or abnormal medical and family history. Endoscopic examination showed bilaterally enlarged tonsils and exudate on left side (Fig. 1), and about 2 ~ 3 cm sized single cervical lymph node was palpated on left side. Her body temperature was 37.3℃, and laboratory findings including absolute neutrophil count and C-reactive protein were checked to 7,510/mm3 and 20.7 mg/L respectively, which indicating active inflammation. Based on these findings, we initially considered that the patient had acute tonsillitis and she was admitted and administered high dose intravenous third-generation cephalosporin plus clindamycin with symptomatic management. About 1 week after her admission, all subjective symptoms were resolved and the laboratory findings also normalized. However, the hypertrophy of the left tonsil and enlarged cervical lymph node remained. Since clinical courses were atypically presented despite administrating antibiotics, we decided to take additional pharyngeal computed tomography scan and fine needle aspiration on cervical lymph node to consider other pathologic conditions.

Endoscopic examination of the tonsil. (A) Enlarged right palatine tonsil, (B) Asymmetrically enlarged left palatine tonsil with exudate on its surface.
The CT scan revealed the asymmetric left tonsillar enlargement and an ipsilateral solitary enlarged lymph node with central low attenuation focus in neck level II (Fig. 2). No purulent material was aspirated during ultrasound-guided fine-needle aspiration. The cytologic report showed no malignant tumor cells but lymphoma can not be excluded and additional excisional biopsy was recommended. With these results, we planned to conduct open excisional biopsy for level II lymph node under general anesthesia, and also the tonsil biopsy if needed.
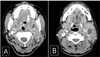
Contrast enhanced computed tomography scan of the patient. (A) Hypertrophic and slightly enhanced left palatine tonsil (white arrow) and (B) Enlarged ipsilateral cervical lymph node which showed central low attenuated lesion (hollow arrow).
The cervical lymph node adhered to the left internal jugular vein, but the dissection was relatively easy, so it was thought to be an inflammatory lymphadenitis. A frozen lymph node biopsy was done during the surgery, but malignancy was not ruled out or confirmed. Thus, a diagnostic left-sided tonsillectomy was also performed for a more accurate diagnosis. The left tonsil which was friable when grasped with forceps adhered to the surrounding tissues. The left cervical lymph node was confirmed to be CD20-positive DLBCL on the final pathological report. The left tonsil was diagnosed with CD20-positive and BCL-6-positive DLBCL (Fig. 3). The patient was discharged without postoperative complications. She was transferred to another hospital for systemic chemotherapy.
DISCUSSION
Our case is about malignant lymphoma misdiagnosed as acute tonsillitis with subsequent cervical lymphadenitis in an adult female. We may have missed the malignant lymphoma if we neglected the residual unilateral tonsillar enlargement with a neck mass after infectious symptoms were subsided.
It is difficult to analyze the incidence and mechanisms of these cases because no similar reports about a malignancy mimicking acute tonsillitis are available. In case of immunocompromised patients, a few studies about head and neck lymphoma confused with acute tonsillitis or a head and neck infections have been reported. Yellin et al. presented a case of tonsil lymphoma presenting as tonsillitis after bone marrow transplantation.8 Berkowitz et al. reported a similar case and insisted that as unilateral tonsillar enlargement progresses, and does not respond to appropriate treatment as in acute tonsillitis, a biopsy is necessary with an immunocompromised and a history of malignant disease.9 Another report demonstrated a patient who had initially been diagnosed with a peritonsillar abscess, but eventually diagnosed as lymphoma in a tonsillectomy biopsy.10
Based on these reports, if our patient had been immunocompromised with unilateral tonsillar enlargement, we planned a biopsy to find a malignancy. However, she had no problematic medical history, and the symptoms and objective findings were nearly resolved after antibiotic treatments and appropriate managements. The clue of another disease was the asymmetric tonsillar enlargement and cervical lymph node enlargement. Fortunately, she received proper treatment for lymphoma.
We experienced a difficult case of malignant lymphoma mimicking acute inflammatory clinical features so that recommend close monitoring if unilateral tonsillar enlargement does not respond and are not resolved with standard antibiotics in an immunocompetent adult patient. Radiological and/or pathological work-ups should be conducted to consider the possibility of a malignant tumor. We consequently report this case to emphasize the importance of a careful evaluation and close follow-up for differentiating malignant lymphoma from an acute infectious disease presenting atypically.
