Gamma Knife Radiosurgery in Recurrent Trigeminal Neuralgia after Other Procedures
Article information
Abstract
Objectives
Trigeminal neuralgia (TN) is undurable paroxysmal pain in the distribution of the fifth cranial nerve. Invasive treatment modalities for TN include microvascular decompression (MVD) and percutaneous procedures, such as, radiofrequency rhizotomy (RFR). Gamma Knife radiosurgery (GKRS) is a considerable option for patients with pain recurrence after an initial procedure. This study was undertaken to analyze the effects of gamma knife radiosurgery in recurrent TN after other procedures.
Methods
Eleven recurrent TN patients after other procedures underwent GKRS in our hospital from September 2004 to August 2016. Seven patients had previously undergone MVD alone, two underwent MVD with partial sensory rhizotomy (PSR), and two underwent RFR. Mean patient age was 60.5 years. We retrospectively analyzed patient's characteristics, clinical results, sites, and divisions of pain. Outcomes were evaluated using the Visual Analog Scales (VAS) score.
Results
Right sides were more prevalent than left sides (7:4). The most common distribution of pain was V1 + V2 division (n = 5) following V2 + V3 (n = 3), V2 (n = 2), and V1 + V2 + V3 (n = 1) division. Median GKRS dose was 80 Gy and the mean interval between the prior treatment and GKRS was 74.45 months. The final outcomes of subsequent GKRS were satisfactory in most cases, and at 12 months postoperatively ten patients (90.0%) had a VAS score of ≤ 3.
Conclusions
In this study, the clinical result of GKRS was satisfactory. Invasive procedures, such as, MVD, RFR are initially effective in TN patients, but GKRS provides a safe and satisfactory treatment modality for those who recurred after prior invasive treatments.
Trigeminal neuralgia (TN) is undurable paroxysmal pain in the distribution of the fifth cranial nerve.12 The most common cause of TN is commonly the compression of the trigeminal nerve by cerebral vessels, but in 3.1%–17% of patients, there is no evidence of neurovascular compression.34 Invasive surgical treatment modalities for TN include microvascular decompression (MVD) or a percutaneous procedure, such as radiofrequency rhizotomy (RFR).
Unfortunately, TN recurs after surgical treatment in some patients.5 Less invasive treatment is common considered initially in recurrent TN because of the risks associated with surgical retreatment, and of the various treatment possibilities, Gamma Knife radiosurgery (GKRS) is considerable an option.678 GKRS provides pain control, by destroying the trigeminal nerve with stereotactic radiation. Some reports have been issued on the efficacy of GKRS in patients with TN, but few studies have addressed the clinical outcomes of patients with recurrent TN after initial surgical treatment treated by secondary GKRS. This study was undertaken to analyze the effects of gamma knife radiosurgery in recurrent TN after other procedures.
MATERIALS AND METHODS
Patients
Eleven recurrent TN patients that underwent GKRS after other procedures at our hospital between September 2004 and August 2016 were enrolled in the present study. The study exclusion criteria applied were initial GKRS and presence of another pathologic condition, such as, a tumor, vascular disease, or multiple sclerosis.
Five of the 11 patients were men. Seven patients had right-sided TN, and 4 left-sided TN. Seven patients had previously undergone MVD, two MVD with partial sensory rhizotomy (PSR), and 2 RFR. Patient characteristics, clinical results, sites, and divisions of pain were analyzed retrospectively. This study was approved by the Institutional Review Board of Pusan National University Hospital (H-1811-009-072).
Pre- and postoperative evaluations
All patients underwent preoperative evaluations, which included magnetic resonance imaging (MRI) with a three-dimensional constructive interference in steady state (3D-CISS) sequence. Clinical outcomes were assessed preoperatively and at 1, 6, 12 and 24 months postoperatively. Outcomes were evaluated using Visual Analog Scales (VAS) score.9 “Pain relief” was defined as VAS score of < 5; “Significant pain relief” was defined as a VAS score reduction of ≥ 5. We also subdivided clinical outcomes at follow-up into 3 categories: good (VAS 0–3), fair (VAS 4–6), and poor (VAS 7–10).
After GKRS, trigeminal nerve sensory dysfunction was categorized by patients as either bothersome or mild.
Radiosurgical Procedures
All procedures were carried out with Leksell Gamma Knife (B. and Perfexion. Elekta, Stockholm, Sweden). Dose planning was performed in all patients using a 0.6 mm axial slice interval with no gap using CISS. Briefly, a Leksell stereotactic coordinate frame was applied to the head under local anesthesia. All patients were treated using a single shot to a prescription dose between 80 and 85 Gy (mean 80.5 Gy) to the maximum dose point using a 4-mm collimator with or without a shield. The Leksell GammaPlan treatment planning system (Eleka) was used to generate treatment plans. The trigeminal target was the root entry zone (REZ) of the TN immediately adjacent to the pons (Fig. 1).
Statistical analysis
The analysis was performed using SPSS 22.0 (SPSS Inc. Chicago, IL, USA). Results are expressed as percentages and the means ± standard deviations. Kaplan-Meier survival curves were plotted for the time to pain relief after GKRS. Statistical significance was accepted for two-tailed P values of < 0.05.
RESULTS
Mean age at the surgery was 60.40 ± 15.31 years (range 39–83 years. Mean preoperative symptom duration was 40.36 ± 28.50 months (range, 6 to 96 months), and mean interval period between the prior treatment and GKRS was 74.45 ± 61.28 years (range 1–182 months). The most common pattern of pain involved both the V1 and V2 distributions of the trigeminal nerve in 5 patients, followed by both the V2 and V3 distributions in 3, the V2 distribution in 2 patients, and all trigeminal distributions in 1 patient. We also evaluated the following clinical characteristics in each group underwent MVD and RFR (Table 1).
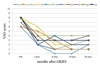
VAS score at each follow-up for individual patients are presented in Fig. 2. Mean VAS scores were 7.55, 3.27, 2.27 and 2.36 pre-GKRS at 1, 6, 12, and 24 months after GKRS, respectively. Pain relief was evaluated using the Kaplan and Meier product-limit method (Fig. 3). “Effective pain relief” appeared early after GKRS, but the “significant pain relief” appeared to be more delayed. Most outcomes at 12 and 24 months after GKRS were satisfactory; 10 (90.9%) and 9 (81.8%) were good, and 1 (9.1%) and 2 (18.2%) were fair, respectively.

Kaplan-Meier estimates of the probabilities of initial pain relief after GKRS
(A) Pain relief (VAS score < 5), (B) Significant pain relief (a VAS score reduction of ≥ 5)
No patient sustained additional sensory disturbances until 6 months after GKRS. At 1-year after GKRS, 4 patients (36.4%) developed in facial paresthesia.
DISCUSSION
TN is caused by extrinsic compression of the trigeminal nerve root entry zone (REZ),110 usually by a normal cerebral vessel. Compressive nerve lesions produce focal demyelination and nerve root distortion,10 and typical TN symptoms include “intense paroxysmal, brief, electric, or stabbing unilateral facial pain along the dermatomal distribution of the fifth cranial nerve”, which serve as the most important diagnostic clues.11
MVD was developed by Jannetta and introduced in the late 1970s, and has become one of the most common treatments for TN with recurrence rates lower than those of other treatments.12 Successful MVD of the TN depends upon the recovery of demyelination after decompression of the REZ. However, some TN patients treated by MVD experience pain recurrence after successful surgery. Many authors have attempted to explain TN recurrence after MVD. Kabatas et al.13 suggested several causes, such as Teflon granuloma formation, excessive Teflon insertion, Teflon dislocation, and post-procedural venous compression.
Hartel first attempted percutaneous rhizotomy of trigeminal nerve divisions in the early 1900s, which was followed later by Sweet in the 1970s using radiofrequency. Hartel's technique describes a method of reaching the gasserian ganglion by passing a needle from the external side corner of the mouth and then passing it inward until the needle tip reaches the temporal bone in front and to the outer side of the foramen ovale (FO).14 This allows the needle to be advanced further into the inner side of the FO to finally reach the gasserian ganglion.15 The success of this procedure is determined by how accurate the needle and electrode are positioned. Gusmão et al.16 proposed recurrences after RFR were due to an inappropriate pathway (not passing the FO) and complications associated with the overall treatment process.
In cases of recurrent TN, reoperation should be considered and less invasive procedures recommended to achieve pain relief for several reasons. First, the success rate of re-operation is significantly lower than that of initial operations. According to previous studies, the success rate of re-operation ranges between 51% and 93.3%.51718 Barker et al.19 reported pain relief in 42% of patients after re-operation, as compared with 64% after initial surgery. The second reason is that the risk of trigeminal nerve injury, and thus, of facial dysesthesia, is higher for reoperation than for initial surgery.
For these reasons, less-invasive treatments are more acceptable for recurrent TN, and GKRS is the most effective and minimally invasive surgical procedure.5202122 Several reports have reported that the success rate of repeat GKRS pain relief is 60–70%.2123 GKRS has been reported to be a relatively complication-free safe method as compared with other procedures, such as, MVD and RFR; the only complications reported to date are dysesthesia or anesthesia dolorasa.24 In this study, we found GKRS substantially improved outcomes in patients with recurrent TN after other procedures with few complications.
This study has several limitations that should be considered. First, it is inherently limited by its retrospective nature. Second, the follow-up (2 years) was relatively short. Third, this cannot completely reflect the pain relief after secondary GKRS because of the small sample size of this study. Therefore, we suggest a prospective, larger-scale study be conducted to confirm the efficacy of secondary GKRS in recurrent TN patients after prior surgical treatment.
In this study, the clinical results of secondary GKRS were satisfactory. Although invasive procedures, such as, MVD and RFR, provide effective initial treatment for trigeminal neuralgia. GKRS appears to be a safe and satisfactory treatment modality for those who recurred after initial or prior invasive treatment.
ACKNOWLEDGMENT
This work was supported by clinical research grant from Pusan National University Hospital in 2018